February 03, 2020
WHO declares 2019-nCoV a global public health emergency. The World Health Organization has declared the novel coronavirus (2019-nCoV) outbreak a Public Health Emergency of International Concern, with at least 17,300 cases of the virus and more than 360 deaths reported across 20+ countries, as of February 3rd, 2020. [WHO]
- In a prospective analysis of 99 2019-nCoV cases in Wuhan, China, researchers found that half of patients had underlying medical conditions, half had contact with the suspected origin of the outbreak (Huanan seafood market), and 11 percent died of multiple organ failure from the virus. Common symptoms include fever, cough, fatigue, and shortness of breath, and 75 percent of patients exhibited bilateral pneumonia. [The Lancet]
- Next-generation sequencing of ten samples from nine infected patients found that 2019-nCoV shares 88 percent sequence identity with two bat-derived coronaviruses, 79 percent sequence identity with severe acute respiratory syndrome (SARS)-CoV, and only 50 percent sequence identity with Middle East respiratory syndrome (MERS)-CoV. [The Lancet]
- Researchers in Beijing estimated that the reproductive number (R0) of 2019-nCoV is higher than that of SARS, at 4.08, while the case-fatality rates of the two viruses are comparable. This R0 estimate is nearly two times higher than the World Health Organization’s estimate of 1.4-2.5, and experts argue that it may be too early on in the outbreak to accurately calculate these numbers. [MedRxiv, CIDRAP]
The benefits of vaccination extend beyond disease prevention. In a new paper, Arindam Nandi, CDDEP Senior Fellow, and Anita Shet at the Johns Hopkins Bloomberg School of Public Health, summarize the broad health, economic, and child development benefits of routine vaccination. While vaccines have long been proven to cost-effectively reduce the burden of disease, recent research has suggested that routine vaccination also improves cognition, schooling attainment, and productivity outcomes in low-income settings. The paper discusses the importance of these policy-informing findings in low-and middle-income countries where the burden of disease is high and resources are limited, as well as high-income countries where vaccine hesitancy is multiplying. [Human Vaccines and Immunotherapeutics]
Repeated antibiotic exposure linked to childhood obesity. A New Zealand cohort study including 5,128 children found that repeated antibiotic exposure in the first four years of life was significantly associated with higher body mass index (BMI) later in childhood. Children who received >9 antibiotic prescriptions by age four were over twice as likely to be obese at age 54 months compared to children with no antibiotic exposure (odds ratio: 2.41, 95% CI [1.07, 5.41]). The authors suggest that future research should evaluate the impact of antibiotic stewardship programs (ASPs) on early childhood obesity. [JAMA Network Open]
Abundance of AMR genes found in dust from indoor settings is low compared to other environments. Researchers from Northwestern University used metagenomics to analyze dust samples from 43 buildings and identified 183 antibiotic resistance genes, which conferred resistance to 15 classes of antibiotics. The study found that 52 of the resistance genes were potentially mobile, meaning that the bacteria could share its genes with its neighbors. However, the abundance of antibiotic resistance genes found in dust from indoor settings was low compared to other environments. [PLOS Pathogens]
Twitterchat on AMR reaches millions. Researchers conducted a case study to assess the impact of a 24-hour “TwitterChat” led by nursing students in creating a global conversation surrounding antimicrobial resistance (AMR). After three days, the “TwitterChat” reached over 2.6 million twitter accounts, and the tweets were seen more than 10 million times. The authors note that they will soon evaluate this impact in a formal study and hope the results will serve as evidence that social media can foster a sense of community and promote the dissemination of AMR information. [Journal of Clinical Nursing]
Mass azithromycin distribution reduces child deaths due to malaria, dysentery, meningitis, and pneumonia in Niger. A cluster-randomized controlled trial in Niger found that biannual mass distributions of azithromycin among children were linked to a decreased incidence of child mortality due to malaria, dysentery, meningitis, and pneumonia (p≤0.05). Between 2014 and 2017, communities in Niger that were randomized to receive biannual mass distributions of azithromycin for children 1-5 years old had one-third fewer child deaths due to meningitis and dysentery (incidence rate ratio: 0.67, 0.65), as well as one-fifth fewer child deaths due to malaria and pneumonia (incidence rate ratio: 0.78, 0.83) compared to communities receiving placebo. [The Lancet Global Health]
New estimates show that sepsis accounts for one in five deaths worldwide. Using data from the Global Burden of Diseases, Injuries, and Risk Factors Study, researchers estimated that in 2017, 48.9 million new cases of sepsis and 11 million sepsis-related deaths occurred worldwide, accounting for nearly one-fifth of all global deaths. Although age-standardized sepsis incidence and mortality decreased significantly between 1999 and 2017 (by 37 and 52.8 percent respectively), the burden of sepsis remains high globally, particularly in sub-Saharan Africa. [The Lancet]
Experimental Ebola vaccine well-tolerated in healthy adults. Researchers conducted a phase 1 clinical trial of a highly attenuated experimental Ebola vaccine (rVSVN4CT1-EBOVGP1) among healthy adults in Melbourne, Florida and evaluated the vaccine as safe and effective in producing an immune response. Of the 39 individuals enrolled in the trial, several experienced local and systemic adverse events that were mild to moderate, including injection site tenderness and fatigue. However, no serious adverse events occurred, and a strong immune response was detected in 100 percent of recipients at all dose levels tested. [The Lancet Infectious Diseases]
Virtual reality may be an effective strategy for improving flu vaccine intentions. Researchers from the University of Georgia and Oak Ridge Associated Universities (ORAU) in Tennessee found that supplementing vaccine information with an immersive virtual reality (VR) intervention was associated with increased influenza vaccine intentions among flu vaccine-avoidant adults. The study found that compared to other educational interventions, VR interventions produced a strong sense of presence in the virtual story, which was linked to an increased understanding of herd immunity as well as an increased intention to receive the flu vaccine. [Vaccine]
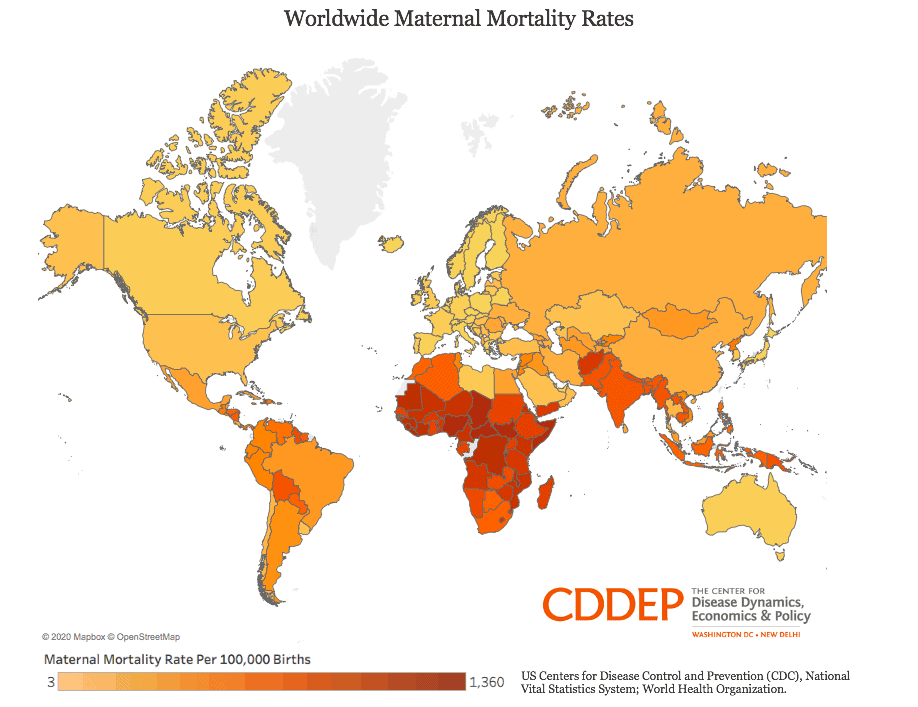
Mothers more likely to die from childbirth in the US than in 10 similarly wealthy countries. [CDDEP, CDC]