July 12, 2024
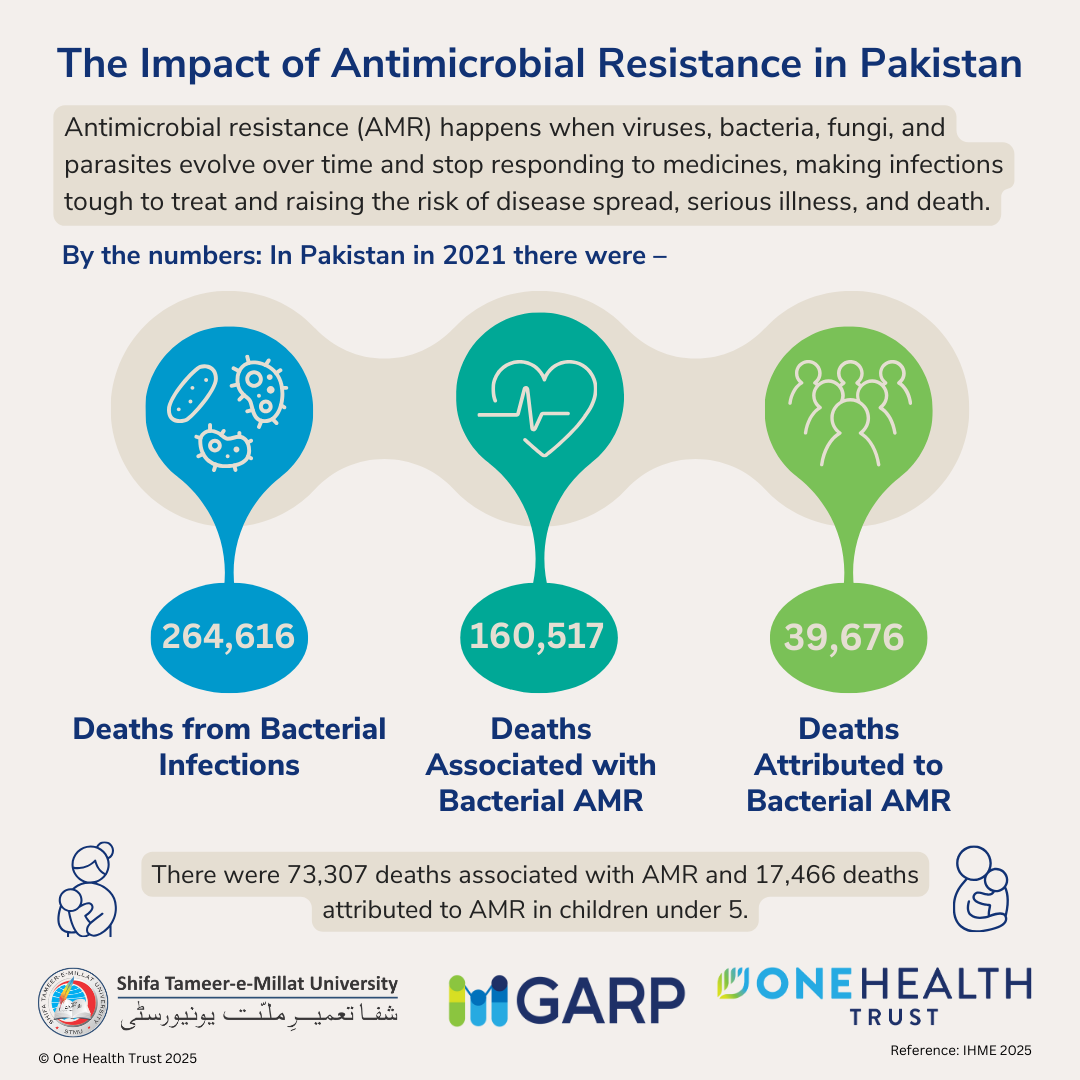
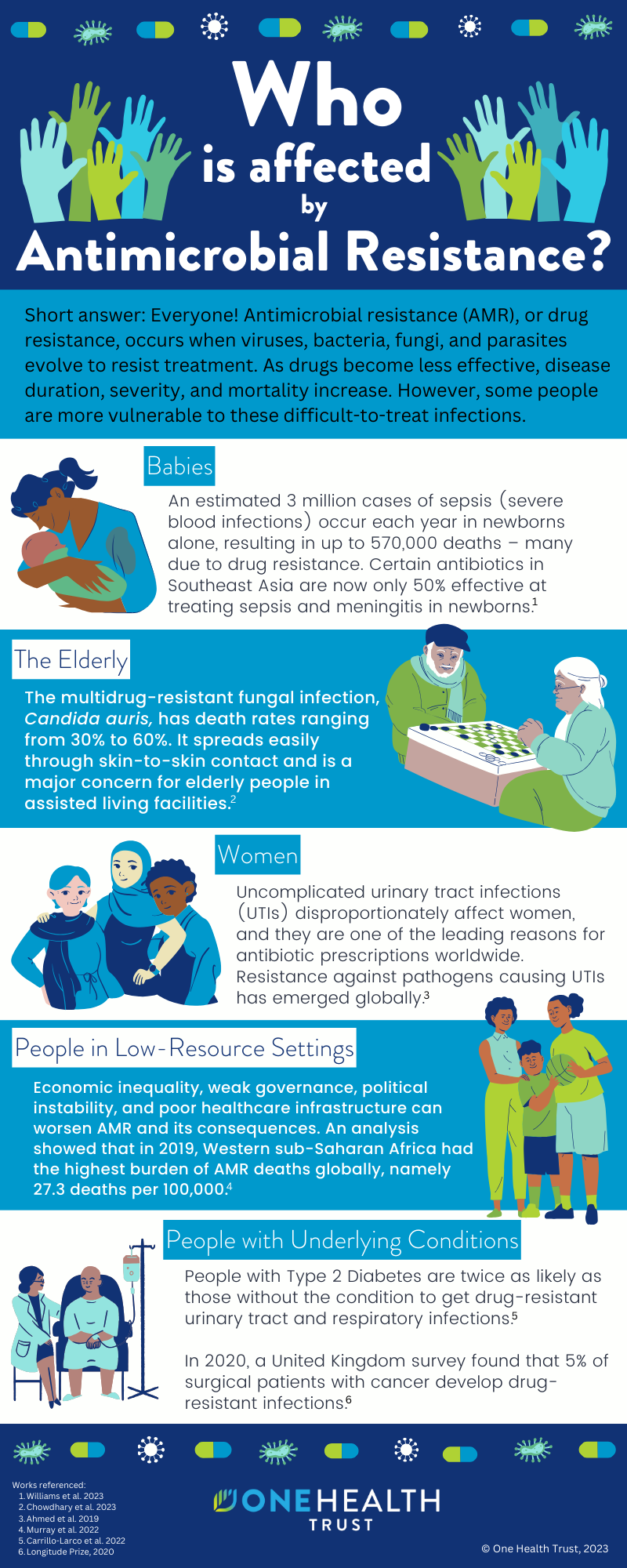
Short answer: Everyone! Antimicrobial resistance (AMR), or drug resistance, occurs when viruses, bacteria, fungi, and parasites evolve to resist treatment. As drugs become less effective, disease duration, severity, and mortality increase. However, some people are more vulnerable to these difficult-to-treat infections.
- Babies: An estimated 3 million cases of sepsis (severe blood infections) occur each year in newborns alone, resulting in up to 570,000 deaths – many due to drug resistance. Certain antibiotics in Southeast Asia are now only 50% effective at treating sepsis and meningitis in newborns.
- The elderly: The multidrug-resistant fungal infection, Candida auris, has death rates ranging from 30% to 60%. It spreads easily through skin-to-skin contact and is a major concern for elderly people in assisted living facilities.
- Women: Uncomplicated urinary tract infections (UTIs) disproportionately affect women, and they are one of the leading reasons for antibiotic prescriptions worldwide. Resistance against pathogens causing UTIs has emerged globally.
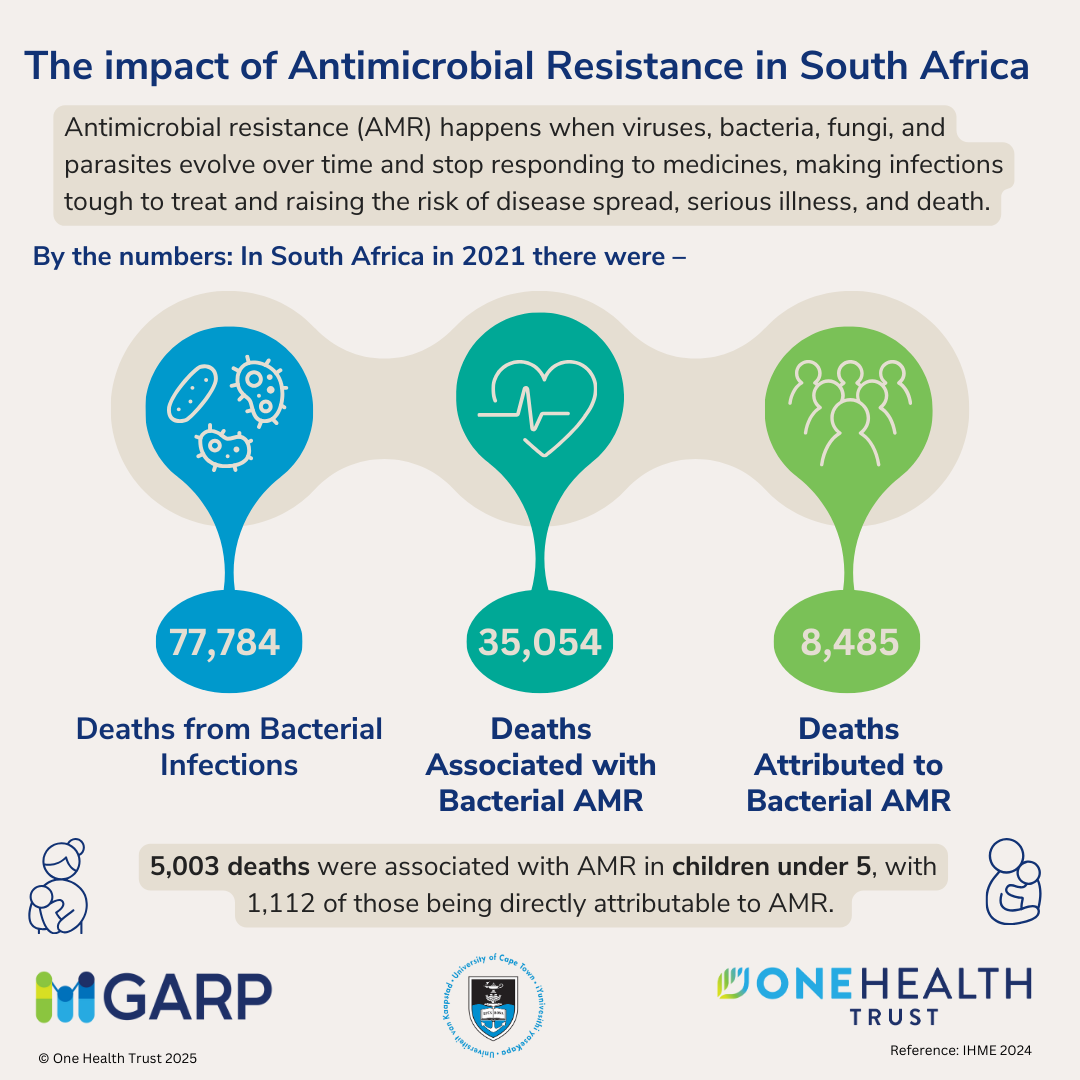
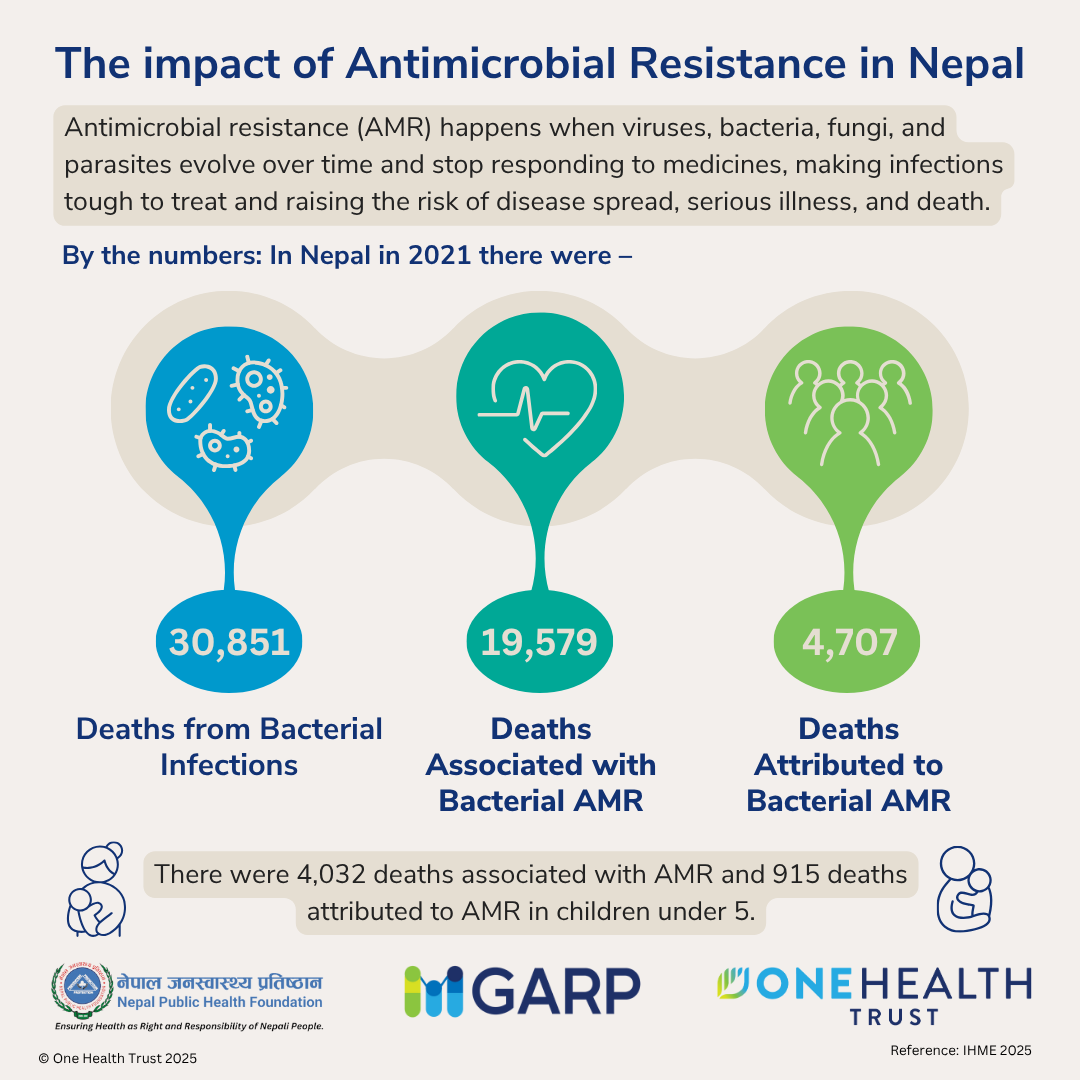
- People in low-resource settings: Economic inequality, weak governance, political instability, and poor healthcare infrastructure can worsen AMR and its consequences. An analysis showed that in 2019, Western sub-Saharan Africa had the highest burden of AMR deaths globally, namely 27.3 deaths per 100,000.
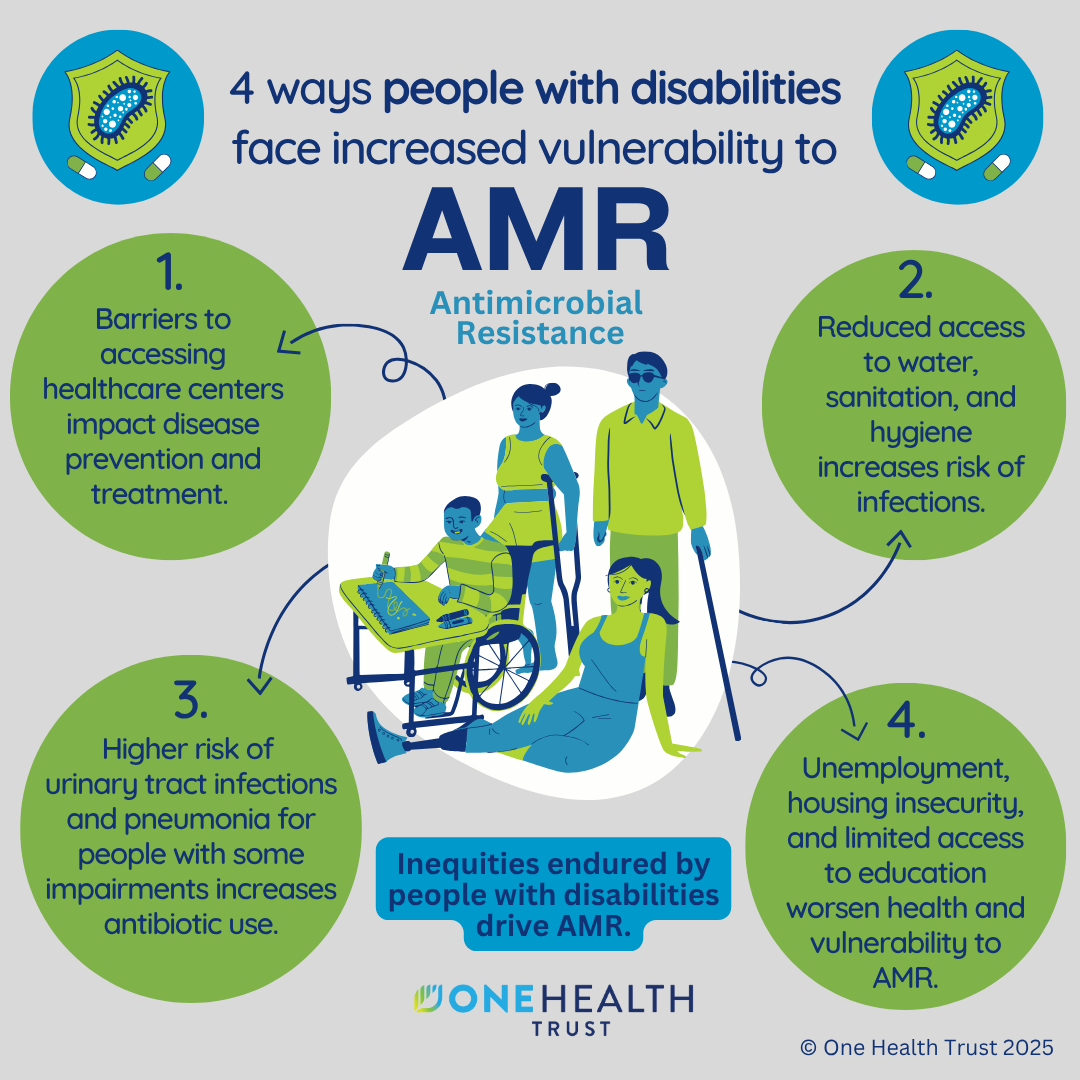
- People with underlying conditions: People with Type 2 Diabetes are twice as likely as those without the condition to get drug-resistant urinary tract and respiratory infections. In 2020, a United Kingdom survey found that 5% of surgical patients with cancer develop drug-resistant infections.