April 28, 2010

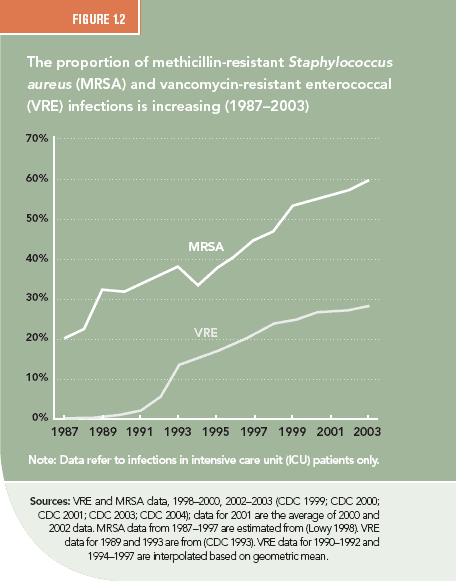
The timeline of emergence of drug resistance is best illustrated by the case of Staphylococcus aureus (S. aureus), a common pathogen that causes life-threatening infections and is transmitted in both health care and community settings. The mortality rate from a S. aureus infection was as high as 82 percent in the preantibiotics era (Skinner and Keefer 1941) but fell dramatically after the introduction of penicillin. Resistance to penicillin emerged soon after its introduction and was linked to patient deaths in the early 1950s (Abboud and Waisbren 1959). In 1960, penicillin was replaced with a beta-lactam compound, methicillin, which was effective against penicillin-resistant S. aureus, but methicillin-resistant S. aureus (MRSA) emerged in the 1970s in Europe and soon after in the United States. MRSA prevalence in U.S. hospitals, which was 2.4 percent in 1975, increased to 29 percent in 1991 (Archer 1998) (Figure 1.2), and 59.5 percent in 2003 (CDC 2004), growing at an average rate of more than 12 percent per year. Vancomycin is the main and potentially last available drug that can reliably treat MRSA infections, and the massive use of vancomycin for treating MRSA is believed to be an important reason for the emergence and spread of vancomycin-resistant enterococci (VRE)(Weinstein 2003). Meanwhile, strains of MRSA resistant to vancomycin have been detected, providing the first glimpse of medical outcomes in a post-antibiotics era (Chang, Sievert et al. 2003).