March 25, 2017
A weekly roundup of news on drug resistance and other topics in global health.
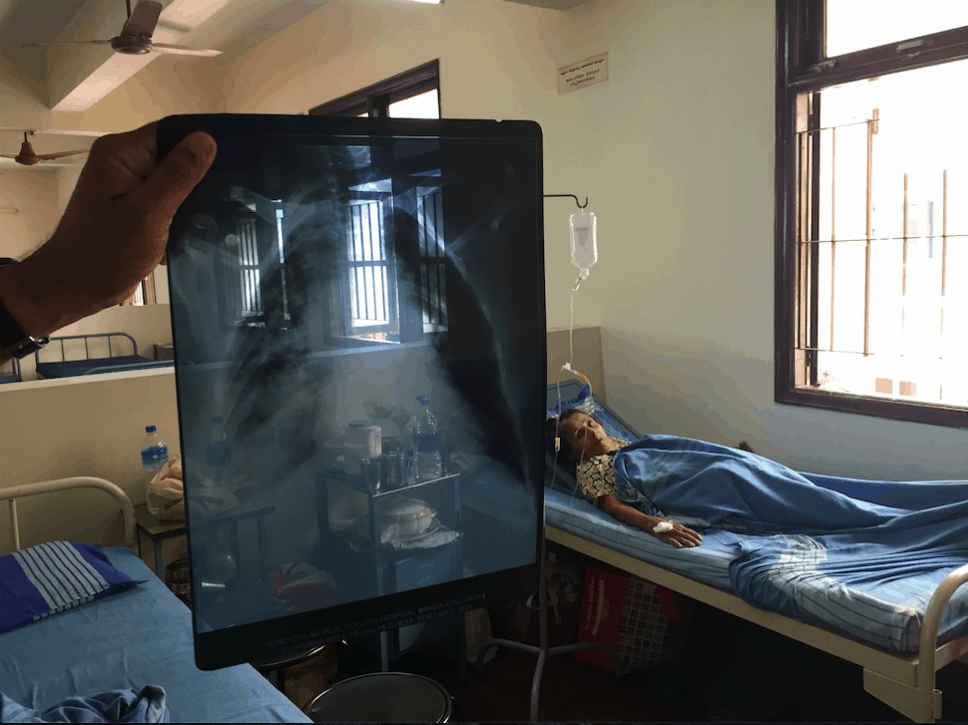
World Tuberculosis Day: disease is globally under-detected, underreported and often untreated. On World TB Day, we recognize the one-third of the global population infected with Mycobacterium tuberculosis, the bacterium that causes TB. Many people lack access to quality treatment and many experience infections increasingly resistant to antibiotics. In an Expert Opinion in The Quint, CDDEP Director Ramanan Laxminarayan writes, “Every year, many new cases are added and unfortunately, many more go undetected. Under-reporting of TB cases has been one of the impediments for effective TB control in India.” [The Quint]
On the CDDEP Blog, Dr. Madhukar Pai, MD, PhD, and Anita Svadzian, MPH, respond to the omission of TB from the World Health Organization (WHO) Priority Pathogens list. While the omission shook public health professionals, WHO defended their decision, asserting that TB is already an established priority. Pai and Svadzian write, “Regardless of the confusion created by WHO, and the missed opportunity to include TB in an important advocacy effort, it is critical to recognize that drug-resistant TB is a key aspect of the global AMR crisis. […] Only about half of patients treated for MDR-TB globally are cured, and the results are substantially worse for extensively drug-resistant disease (XDR-TB).”
Dr. Pai also has an editorial in The Lancet, “Reducing global tuberculosis deaths—time for India to step up,” naming India, with one quarter of the world’s cases, as “ground zero” for the epidemic. [CDDEP Blog, The Lancet]
UN launches ethics guidance to protect rights of TB patients and address stigma, discrimination. The United Nations has released an ethics guidance to ensure that countries implementing the WHO End TB Strategy maintain ethical standards in treating the affected. The guidance stresses these overarching goals and values:1) ending TB as a matter of social justice, 2) ethics and human rights: key foundations of the End TB Strategy, 3) guiding principles and values to help end TB, and 4) the obligation to provide access to TB services. According to Director of the WHO Global TB Programme Dr. Mario Raviglione, “Only when evidence-based, effective interventions are informed by a sound ethical framework, and respect for human rights, will we be successful in reaching our ambitious goals of ending the TB epidemic and achieving universal health coverage.” [WHO press release, WHO Ethics Guidance]
Lancet Infectious Diseases editorial responds to WHO Priority Pathogens list. An editorial in Lancet ID, “Antibiotic research priorities: ready, set, now go,” addresses the WHO’s recently published list of pathogens that pose the greatest risk to the global population and suggests that setting priorities has its drawbacks. According to the editorial, the omission of TB “risks weakening any sense of urgency,” for the development of new treatments. The authors note that TB was not the list’s only omission—Clostridium difficile is responsible for a large burden of disease and is in need of new narrow-spectrum antibiotics. The editorial concludes, “The top priority now for antimicrobial research and development is not A baumannii, S aureus, or MDR-TB. It is to find a way to bring together pharmaceutical companies, governments, civic society, and academics to overcome decades of stagnation, to stimulate research, and to generate some effective new medicines.” [Lancet ID]
Reviewing even negative urine test results in urgent care settings can significantly reduce antibiotic use. While it is a standard practice to prescribe antibiotics in children with acute infections, reviewing negative test results to guide treatment can have a significant impact on antibiotic use, especially in urgent care settings. A new study published in the journal Pediatrics, finds that following a standard protocol for review of negative infection test results led to discontinuation of antibiotic use in 80 percent more cases than usual. Researchers at the Nationwide Children’s Hospital (NCH) in Ohio followed up more than 900 pediatric cases of urinary tract infections at a network of urgent care centers, implementing a standardized protocol for follow-up management on negative urine culture results. The study also found a 40 percent decrease in antibiotic days in these patients. This demonstrates that even a negative urine test result can be useful in guiding antibiotic use in urgent care settings. The authors suggest this as an important target area for antibiotic stewardship that should be further studied, including in outpatient settings. [Pediatrics, CIDRAP]
FAIIR and ShareAction progress report: Coordinated investor and consumer push for prudent use of antibiotics in livestock yields results. Food and poultry companies have a history of using low-dose antibiotics for growth promotion and disease prevention in livestock, which contributes to rising antimicrobial resistance (AMR) in humans. Knowing that companies respond to public pressure, the FAIRR (Farm Animal Investment Risk and Return) initiative and Share Action brought together a $1 trillion group of investors one year ago to engage with 10 of the world’s largest restaurant and fast-food chains, urging them to reduce their antibiotic use. After one year, they report substantial progress in reducing antibiotic use in poultry by companies such as McDonald’s, but little change in beef and pork practices. They continue to gain collaborating investors, and urge companies to set timelines for phasing out antibiotic use. [FAIRR report]
Impact of antibiotic stewardship programs in fighting quinolone resistance: A systematic review in Advances in Therapy evaluates the impact of stewardship interventions on quinolone resistance rates and healthcare-associated infections (HAIs). The analysis resulted in recommendations for improvements in quinolone-targeted stewardship programs, including restrictive policies, prospective audits with feedback to prescribers, infection prevention and control measures, prompt detection of low-level resistance, educational programs, and guidelines for optimal use. The article suggests that these interventions would be strengthened by novel approaches in diagnostic stewardship for rapidly detecting bacterial resistance, including mass spectrometry, microarrays, and whole-genome sequencing. [Advances in Therapy]
Efficacy of low-cost, heat-stable oral rotavirus vaccine in Niger: A study in the New England Journal of Medicine reports on the efficacy of a heat-stable oral rotavirus vaccine in Niger. Rotavirus is a leading cause of severe gastroenteritis among young children and is responsible for about 37 percent of deaths from diarrhea among children under five years. Sub-Saharan Africa currently has the highest rate of rotavirus-associated death, but faces barriers to vaccination with the two vaccines currently meeting WHO prequalification, including high prices, a limited global supply, and unreliable transportation and storage. The vaccine evaluated in this study is heat stable and set at or below the current price of the two WHO prequalified vaccines. The trial involved 3,508 infants randomized to either the BRV-PV vaccine or placebo, in 2014-2015. BRV-PV vaccine efficacy was 70 percent for severe episodes of rotavirus gastroenteritis. Efficacy rates in trials of other rotavirus vaccines in Europe and Latin America are higher (80.5 to 90.4 percent), a differential seen for many vaccines between richer and poorer populations. [NEJM]
Image courtesy of Dr. Madhukar Pai











