March 03, 2017
A weekly roundup of news on drug resistance and other topics in global health.
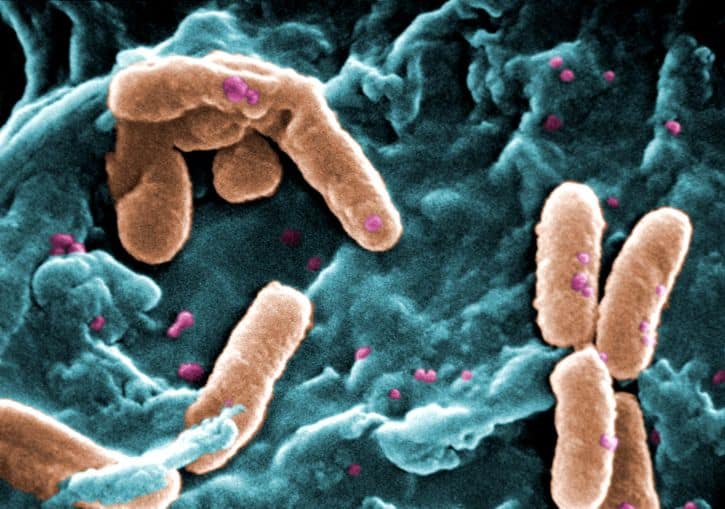
World Health Organization: 12 priority pathogens “pose the greatest threat to human health.” The World Health Organization (WHO) has listed 12 types of antibiotic-resistant bacteria that pose the greatest threat to human health and require urgent research and development for new antibiotics. In the highest priority category—“critical”— are multidrug-resistant Gram-negative pathogens that occur mainly in hospitals and other facilities, specifically Acinetobacter baumannii, Pseudomonas aeruginosa, and species in the Enterobacteriaceae family. The remaining pathogens are classified as “high” and “medium” priority. According to WHO Assistant Director-General Dr. Marie-Paule Kieny, “This list is a new tool to ensure R&D responds to urgent public health needs. Antibiotic resistance is growing, and we are fast running out of treatment options. If we leave it to market forces alone, the new antibiotics we most urgently need are not going to be developed in time.”
The list excludes tuberculosis because, according to WHO, it is “targeted by other, dedicated programmes.” WHO affirmed the gravity of the growing problem of multidrug-resistant tuberculosis in another statement on Tuesday, however. An estimated 580,000 cases and 250,000 deaths due to multidrug-resistant TB (MDR-TB) occurred globally in 2015. Only two new antibiotics to treat MDR-TB have completed phase 2B trials in the past 50 years and both are currently in phase 3 trials. [WHO Priority Pathogens, WHO Tuberculosis Statement, CIDRAP
In U.S., multidrug-resistant infections rising in children. A study in the Journal of the Pediatric Infectious Diseases Society finds that multidrug-resistant Enterobacteriaceae has risen significantly in U.S. children (under age 18) between 2007 and 2015. Data from 48 children’s hospitals across the country were examined for Enterobacteriaceae infections, which include the Gram-negative bacteria Salmonella, Escherichia coli, and Klebsiella. More than 100,000 hospital discharges over the eight-year period involved Enterobacteriaceae diagnoses, with the greatest number caused by E. coli urinary tract infections The proportion of Enterobacteriaceae infections that were multidrug-resistant rose more than seven-fold, from 0.2 percent in January 2007 to 1.5 percent by March 2015. Lead author Sharon Meropol, MD, PhD, told CIDRAP News, “There are very few antibiotics that can treat these bacteria….The main thing is to be really, really careful with how we use antibiotics, and not use them in ways that we know they are really unlikely to be a benefit.”[JPIDS, CIDRAP]
For H7N9 avian influenza, resistance arose after treatment. China is currently in its fifth wave of H7N9, with cases reported from mainland China reaching at least 460, the largest number since the virus appeared in 2013. About 7 percent of human H7N9 cases contain genetic markers for resistance to neuraminidase-inhibiting antivirals such as oseltamivir (Tamiflu) and zanamivir (Relenza). The WHO believes that resistance likely arose after treatment of human cases of H7N9 with the antivirals, as the mutation has not been identified in any poultry samples and in only one environmental sample. H7N9 recently transitioned from a low-pathogenic to highly-pathogenic form of the virus in birds, though WHO officials maintain this would not affect pathogenicity and transmissibility in humans. [STAT, WHO audio, CIDRAP]
In UK, minority of patients receive majority of antibiotics. A UK study has found that half of antibiotics prescribed to adults in primary care were given to less than 10 percent of patients, The study, published in the Journal of Antimicrobial Chemotherapy, is based on electronic health records from nearly two million adults registered with 385 primary care practices in the UK from 2011–2013. Thirty percent of patients were prescribed at least one antibiotic per year, with 9 percent of patients prescribed 53 percent of the total amount of antibiotics, receiving at least five antibiotic prescriptions over three years. Comorbidities increased the prescribing rate by 44 percent and rates of prescribing to women exceeded those in men by 62 percent.
The UK has seen a 40 percent rise in the use of colistin, a last resort antibiotic, from 2014 to 2015, in highly-resistant infections, according to The Bureau of Investigative Journalism. Despite global pressure to eliminate or greatly reduce the use of colistin in farm animals, the UK government licensed three new colistin products last year for use on British farms. Professor Timothy Walsh, one of the discoverers of colistin resistance, calls this “sheer, utter madness.” [JAC, TBIJ]
Experts call for antibiotic resistance educational materials specific to LMIC contexts. “Targeted educational content might be most important for resource-limited settings. In response to this need, we are collaborating to develop online educational templates suitable for adaptation by individual countries based on their clinical needs, practical circumstances, and native language.” In their comment in The Lancet Infectious Diseases, the authors describe stewardship training modules, currently in development by WHO, that will address three areas of focus: stewardship education, improvement of clinical microbiology and reporting, and (pharmaceutical) regulatory interventions. [Lancet ID]
NIH Open Science Prize winner Nextstrain.org tracks evolution of pathogens in real time. Nextstrain.org is a prototype online platform created by Real-time Evolutionary Tracking for Pathogen Surveillance and Epidemiological Investigation to track the evolution and spread of global pathogens in real time. The tool pools data from across the globe to perform rapid phylogenetic analysis and present an online visualization of geographic spread, timings of introduction events, and connected cases. The Open Science Prize is sponsored by the National Institutes of Health, in collaboration with the Wellcome Trust and the Howard Hughes Medical Institute (HHMI). [NIH, Nextstrain.org]
Discovery Awards from the Longitude Prize provide seed funding to advance diagnostics ideas. For teams facing financial barriers to submitting an application for the Longitude Prize, the competition has launched the Discovery Awards, with small grants of up to £25,000. The awards are intended to help teams pay for inputs critical to moving their ideas into products. The grants are open to all registered Longitude Prize teams. The deadline to register for the Discovery Awards is April 21. [Discovery Awards]











