March 17, 2017
A weekly roundup of news on drug resistance and other topics in global health.
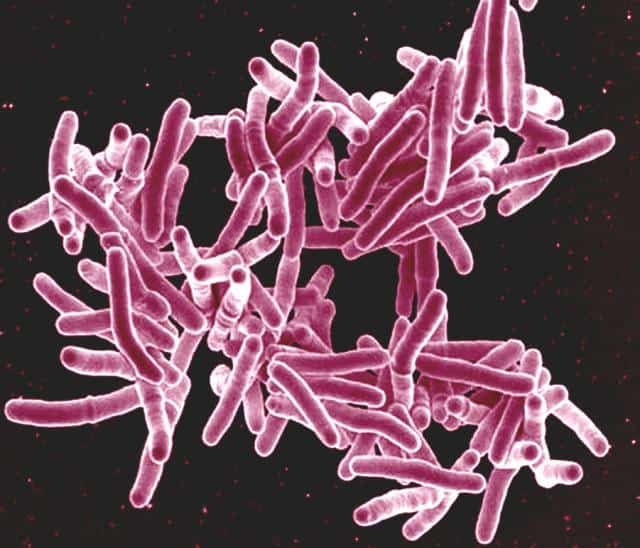
New approach estimates tuberculosis burden in India, models transmission dynamics of urban and rural regions. The extent of tuberculosis in high-burden regions is difficult to measure directly, but it may be possible to estimate TB incidence in other ways. A new study from CDDEP and partners has developed an approach to estimate the extent of TB in India using previous estimates from nearby countries and a current understanding of TB transmission, published in The International Journal of Tuberculosis and Lung Disease. The study also finds differences in urban and rural TB dynamics, specifically the number of people likely to be infected by a single patient and the length of time that patient remains infectious. An urban TB case will infect an average of 12 people per year and remain infectious for about one year, while a rural case will infect an average of 4 people per year, but remain infectious for more than two years. Improved estimates of TB incidence in India and a deeper understanding of transmission dynamics are necessary to develop effective strategies for control. [International Journal of Tuberculosis and Lung Disease]
New study from CDDEP and Resources for the Future examines structured expert judgment—a technique for using expert judgment as scientific data.The study in Reliability Engineering & System Safety updates the 2008 TU Delft structured expert judgment database, which allows researchers to score the accuracy of expert judgment and validate schemes for combining judgments The study also cross-validates the performance of the Classical Model of aggregation used by the 2008 TU Delft database relative to other aggregation models. [Reliability Engineering & System Safety]
UN launches Interagency Coordination Group on Antimicrobial Resistance. The United Nations has launched an interagency coordination group to provide practical guidance on global action to address AMR. The mandate for the group comes from the Political Declaration of the High-Level Meeting on Antimicrobial Resistance, adopted by Member States in September 2016. Deputy Secretary-General Amina Mohammed and Margaret Chan, Director-General of the World Health Organization (WHO), will co-chair the Coordination Group, whose members will be high-level representatives from relevant UN agencies, other international organizations, and individual experts across sectors of animal health, agriculture and environment. WHO, the UN Food and Agriculture Organization (FAO), and the World Organisation for Animal Health (OIE) joined in the launch. [WHO]
Serious fungal infection reported in United States. Candida auris, a yeast that causes serious, highly drug-resistant bloodstream infections, has sickened nearly three dozen people in the United States. It first emerged in 2009, and has been reported from Colombia, India, Israel, Kenya, Kuwait, Pakistan, South Korea, Venezuela and the United Kingdom. The strain mainly infects patients with other serious medical conditions. No “homegrown” strains have appeared in the United States, and according to the CDC’s top fungal expert Tom Chiller, this “gives [the United States] a better opportunity to contain it and stop it from spreading.” Antifungal resistant infections are often included in antimicrobial stewardship discourse, and Chiller adds, “This is a paradigm shift, because Candida is not generally thought of as highly resistant or passed person to person.” [The Washington Post]
Lancet GH commissions report on strengthening quality of care in LMICs. The Lancet Global Health Commission on High-Quality Health Systems in the SDG Era will bring together 30 experts and policymakers from 18 countries to report on improving the quality of primary health care facilities in low- and middle-income countries. The Commission will “review current knowledge, undertake new empirical work, and propose policy recommendations for measuring and improving quality in pursuit of the SDGs. It will produce a single conceptual framework of high-quality health systems to increase the salience of the concept to policymakers, providers, and people.” Commission working groups will consider “ethical dimensions of quality, including the right to quality health-care and equity” in their deliberations. Improving the quality of care, particularly at the primary care level, is a needed step toward achieving the Sustainable Development Goals [Lancet GH]
Mobile phone-delivered reminders may improve childhood immunization. A study published in The Lancet Global Health suggests that short message service [SMS] reminders and monetary incentives can improve immunization uptake. Researchers conducted a trial in 152 villages in Kenya, involving 2018 caregivers and their infants, allocated to four groups: control, SMS reminder only, SMS plus 75 Kenya Shilling (KES) incentive, and SMS plus 200 KES (85 KES = USD$1). Of 2018 caregivers, 1,600 children were successfully followed up and 1,375 (86 percent) achieved full immunization by 12 months of age. The highest overall coverage occurred in the group receiving an SMS and 200 KES incentive, though a significant increase was measured across all intervention groups. According to the authors, global immunization coverage levels have stagnated around 85 percent and this might be one way to reach the remaining 15 percent. [Lancet GH]
A test for TB cure would reduce the incidence of antibiotic resistance. In an extended interview with The Conversation Africa, Dr. Gerhard Walzl, Head of the Immunology Research Group at Stellenbosch University’s Division of Molecular Biology & Human Genetics, describes the long and difficult treatment regimen for TB, which often leads to drug-resistant disease. Most—80 to 85 percent—of patients are cured with courses shorter than the standard six-month treatment, but we have no way of knowing which patients are cured and which require the full six months. If patients with remaining infection stop treatment early, they risk an even more difficult-to-treat, resistant infection. The Predict-TB consortium, with research groups in South Africa, China, and Europe, are developing treatment-stopping criteria based on lung scans, as well as a point-of-care device to measure biomarkers of cure so that treatment can be safely stopped when cure is achieved. If they are successful, patients will benefit directly by avoiding months of difficult treatment, and the rest of the world will benefit from reduced resistance to TB drugs. [The Conversation Africa]
Image via NIAID











