April 07, 2017
A weekly roundup of news on drug resistance and other topics in global health.
Experts say, “Antibiotic-resistant ‘superbugs’ are here.” Antimicrobial resistance has loomed for decades amid inaction and loose regulation, while antibiotic use has soared and the pace of pathogen evolution accelerated. In a Council on Foreign Relations expert brief, Laurie Garrett, CFR Senior Fellow for Global Health, and CDDEP Director Ramanan Laxminarayan discuss the emergence of plasmid-mediated resistance, the recent wave of coordinated global action, and policy work yet to be done. They write, “Rising antimicrobial resistance (AMR) is a classic long-tail problem; it presents a grim ultimate prospect that is reached incrementally over a long period of time. […] Yet other crises always loomed with greater immediacy, pushing AMR to the political back burner.” [CFR]
At SDRI 2017, Laxminarayan evokes future of political action against AMR. Professor Laxminarayan addressed the Solutions for Drug-Resistant Infections (SDRI 2017) conference about maintaining and leveraging the momentum achieved through the UN High-Level Meeting on Antimicrobial Resistance by developing realistic goals, stimulating political will, mobilizing resources, and creating an accountability mechanism for global collective action against AMR. Dame Sally Davies, UK Chief Medical Officer, Tim Jinks, Head of Drug-Resistant Infections at the Wellcome Trust, and other global leaders also addressed the conference [ID Hub]
Translating political commitment into national action on AMR. An editorial from the World Health Organization (WHO) poses the next challenge in the fight against antimicrobial resistance: translating political momentum into policy action at the country level. Substantial progress has been made since the WHO Global Action Plan on Antimicrobial Resistance launched in May 2015 and the United Nations General Assembly held its High-Level Meeting on Antimicrobial Resistance in September 2016, But the toughest part is yet to come: implementing effective policy at the country level and scaling up antimicrobial stewardship and surveillance policies that are already in place. [WHO]
In South Asia, antimicrobial use in agriculture gains industry attention. At VIV Asia, an international agricultural trade show, this year’s theme was antimicrobial reduction. Sasi Jaroenpoj, DVM, of the Thai Department of Livestock Development (DLD) spoke of the need for cooperation between the private and public sectors to track and trace the sale of medicated feed domestically and across borders. Sasi explained, “The lack of restrictions on medicated feed production, the high concentration of medicated premixes, including the uncontrolled access to antibiotics without veterinary oversight, could drive antimicrobial resistance rates in Asia higher than in Europe.” Alternatives to antibiotics for promoting growth and keeping animals healthy were featured by many speakers. [Bangkok Post, PigProgress]
“BashtheBug” citizen science project launched to study antibiotic resistance in tuberculosis. In this “citizen-as-researcher” project, volunteers are shown wells with bacterial growth medium that have been seeded with Mycobacterium tuberculosis and varying doses of an antibiotic. Observers are asked to pick out wells with multipying bacteria. BashtheBug is part of the CRyPTIC project, which is collecting and analyzing more than 100,000 TB infection samples until 2020. According to Dr. Philip Fowler, lead researcher, “Knowing which antibiotics are effective against a particular bacterial infection is crucial for effectively treating a patient, while also limiting the opportunity for the bug to develop antibiotic resistance… Cultivating and examining TB plates is a time-consuming process, but by enlisting extra help online we hope to examine over 40 million images, something we could never do on our own.” [Bash the Bug, Wellcome Trust]
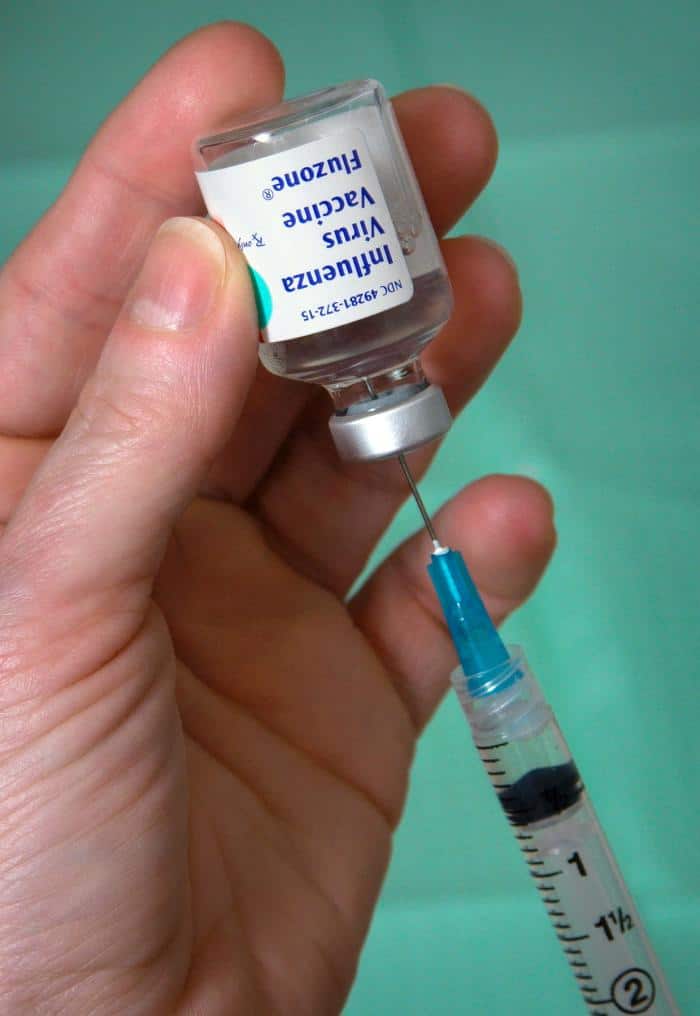
Seasonal flu vaccine prevents child deaths. A CDC study published in the journal Pediatrics finds vaccines can help prevent at least half of influenza deaths in children with underlying medical conditions and is at least 65 percent effective in children with healthy immunity. “That’s very important information to have, especially for families of high-risk kids,” said lead author and epidemiologist in the Influenza Division at the CDC, Brendan Flannery. The study considered laboratory-confirmed influenza cases over four years and studied the effectiveness of the vaccine at different times, including seasons with mild flu, severe flu, and seasons with H1N1 or H3N2. The vaccine was found to be effective at preventing deaths in all of these seasons. This is the first study focused on children supporting the effectiveness of flu vaccines in preventing flu-related deaths. [CIDRAP, Pediatrics]
Russia commits funding to promote food safety and prevent antimicrobial resistance in food and on farms. Russia has committed $3.25 million toward the United Nations Food and Agriculture Organization’s (FAO) fight against rising antimicrobial resistance (AMR) in food and on farms. The project is operational in Armenia, Belarus, Kazakhstan, Kyrgyzstan, and Tajikistan. The aims are 1) to strengthen legal and regulatory measures and develop national response plans to prevent AMR from spreading, 2) to increase the awareness levels among stakeholders and 3) to build surveillance systems to monitor AMR in agriculture and food chains. Commending Russia for the support, FAO Deputy Director-General Maria Helena Semedo said, “AMR is intimately connected to health, medical care, safe food production systems, and the environment. Leaving AMR unchecked would leave a dim vision of the future.” [CIDRAP, FAO]
Infectious Disease Reports special issue, “Integrated Antimicrobial Stewardship: an easy approach to a complex challenge?” A special issue of Infectious Disease Reports features articles on sustainable financial support, multi-professional education, and many other facets of antimicrobial stewardship. The collection includes the article, “Linking sustainable use policies to novel economic incentives to stimulate antibiotic research and development,” in which Ursula Theuretzbacher, Christine Årdal, and Stephan Harbarth discuss the need for new economic models that focus on rewarding innovation while building in provisions for access and sustainable use. [Infectious Disease Reports issue, article]
Image via CDC











