May 05, 2017
A weekly roundup of news on drug resistance and other topics in global health.
Do small community hospitals have lower AMR rates than large tertiary care hospitals? A study from CDDEP researchers finds that may not be the case in the United States. In a study published in Clinical Infectious Diseases, CDDEP researchers find that rates of antimicrobial resistance (AMR) are similar between large tertiary care hospitals and small community hospitals, considering inpatients and outpatients combined. Using a national antimicrobial susceptibility database, researchers compared annual and aggregated rates from community and tertiary care hospitals from 1999 to 2012 for multidrug-resistant Escherichia coli, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa. After accounting for time trends and hospital-level variability, there was no significant overall variation between the two settings. Some differences were noted in comparisons of inpatients—S. aureus, K. pneumoniae, and A. baumannii AMR rates were higher in small community hospitals and in outpatients, rates of AMR S. aureus and P. aeruginosa were higher in tertiary care outpatient settings. A clear increasing trend of AMR in both settings and all pathogens was further confirmation of a growing national problem. The authors conclude that these trends, particularly in AMR E. coli, indicate a continued need to improve infection control and antimicrobial stewardship in all settings. [Clinical Infectious Diseases]
Rethinking narratives we use to explain antimicrobial resistance and stewardship: Commenting in Nature, leaders in discourse surrounding AMR call on the global health community to rethink the language it uses to describe AMR to the public and urge the United Nations Interagency Group on AMR to coordinate a review of terminology. Many surveys confirm the public’s lack of familiarity with the language of AMR, which translates to a lack of appreciation for its seriousness. The authors favor the term “drug-resistant” and suggest that words such as “antibiotic” and “antifungal” be used in preference to “antimicrobial” when referring to a specific type of organism. The authors also argue against narratives of “fight” and conflict, writing, “War and threat were once potent rallying calls. But a more nuanced, balanced, standardized vocabulary is now needed — one that takes ecological balance into account.” [Nature]
Antibiotic use in pregnancy associated with higher miscarriage risk: A study in the Canadian Medical Association Journal finds that pregnant women may be at a higher risk of miscarriage if exposed to certain antibiotics during gestation. Researchers examined the records of more than 95,000 pregnant women in Quebec, finding that use of macrolides (except erythromycin), quinolones, tetracyclines, sulfonamides, and metronidazole was associated with between a 65 percent to two-fold increase in risk of miscarriage in early pregnancy, and norfloxacin associated with a nearly five-fold increase in risk. Not linked to increased miscarriage risk was exposure to nitrofurantoin, erythromycin, penicillins, and cephalosporins. The authors note that these findings are consistent with previous studies indicating an association between antibiotic exposure and increased risk of miscarriage, but acknowledge that in this study, they were not able to fully adjust for severity of infection as a confounding factor, which could have influenced the chance of miscarriage. The authors suggest that these findings “may be of use to policy-makers to update guidelines for the treatment of infections during pregnancy.” [CMAJ, CIDRAP]
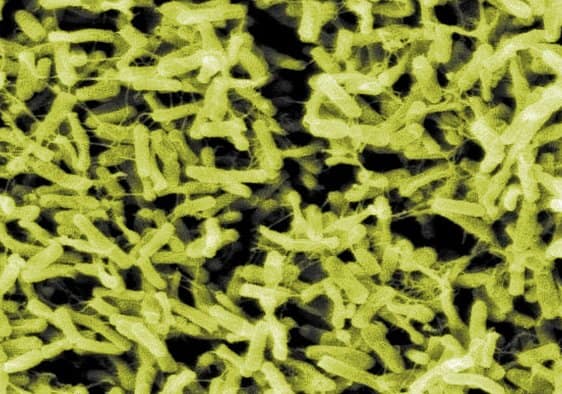
Promising new drug for C. difficile: In a phase 2 study published in The Lancet Infectious Diseases, ridinilazole, a new drug candidate for treating Clostridium difficile infection (CDI), was more effective than vancomycin. CDI usually occurs with long-term use of antibiotics, triggering a severe form of antibiotic-associated diarrhea. Currently, drug treatment options are limited to just three: metronidazole, vancomycin and the newest and possibly most effective, fidaxomicin. Resistance to metronidazole is already rising and is an inevitable consequence of use for all antimicrobials. In this small trial, two-thirds of patients taking ridinilazole versus 44 percent of those taking vancomycin had a sustained clinical response in a combined measure of cure and recurrence prevention. The results clearly support a large phase 3 trial. [Lancet ID]
New antibiotic resistance gene in cow’s milk bacteria: Researchers in Switzerland have identified a new antibiotic resistance gene called mecD in Macrococcus caseolyticus, a common bacterium of cows, often found in the milk of cows with mastitis, infection of the udder. mecD codes for resistance to all b-lactam antibiotics, including penicillin and last-generation cephalosporins used to treat infections like methicillin-resistant Staphylococcus aureus (MRSA). Researcher Vincent Perreten from the University of Bern said, “So far, we do not have any indication of the presence of mecD in humans, but its transfer from M. caseolyticus to S. aureus would further limit therapeutic options of this pathogen. It is imperative to keep an eye on the evolution and spread of this novel resistance gene in both human and animal bacteria.” [India Today, Biospectrum]











