August 20, 2016
A weekly roundup of news on drug resistance and other topics in global health.
CDDEP Director Ramanan Laxminarayan recommends hard targets, funding, and governance to combat AMR, in advance of a United Nations General Assembly (UNGA) High-Level Meeting on Antimicrobial Resistance on September 21, 2016. In Science, Laxminarayan and co-authors explain that without specific targets, adequate financing, and an effective One Health governance structure, the resolution expected to emerge from the UNGA session may have little lasting impact. One target would be reducing national per capita antibiotic consumption to the current global median (8.5 defined daily doses per year) in every country, which would reduce global use by 18 percent. [Science, CIDRAP]
Cost, benefits and obstacles to antimicrobial resistance surveillance in low- and middle-income countries assessed in CDDEP-led World Bank case study. Antimicrobial resistance (AMR) surveillance is key to understanding patterns and trends in AMR, but few low-resource countries have begun surveillance programs. CDDEP Associate Director for Policy Hellen Gelband and colleagues from Nigeria and Kenya assessed the East Africa Public Health Laboratory Networking Project (EAPHLN) experience for a World Bank case study on Strengthening the Role of Laboratories in Tracking Antimicrobial Drug Resistance in East Africa, released this week. Despite significant World Bank support and upgraded facilities, bacteriology lags behind other functions in EAPHLN labs, which conduct few of the antibiotic susceptibility tests that form the basis of AMR surveillance. The case study identifies obstacles to better performance and issues a series of recommendations, which have wide applicability in low- and middle-income countries around the world. It also reviews AMR surveillance programs around the world, their organization, costs and benefits. [CDDEP]
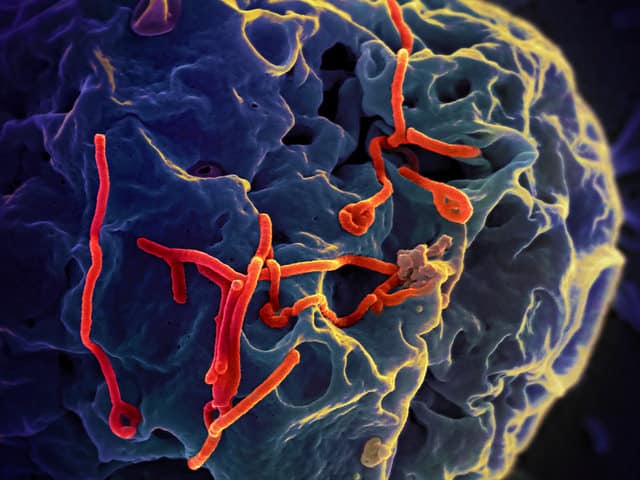
Ebola victims were 20 percent more likely survive if they also had a malaria infection. The study in Clinical Infectious Diseases, led by researchers from the U.S. National Institutes of Health, was carried out in Liberia. Blood samples from 1,868 suspected Ebola patients were tested and 1,182 were confirmed. Of these, 956 were tested for malaria, and 185 were positive for the Plasmodium parasite. Survival was 58 percent for patients with both infections and 46 percent for those with Ebola alone, a 20 percent increase in survival that was independent of treatment with antimalarials. The finding could lead to a better understanding of Ebola pathology and possibly new treatments. [Clinical Infectious Diseases, Los Angeles Times]
FluMist vaccine shown to be as effective as the injected inactivated vaccine, contradicting June recommendations of the CDC’s Advisory Committee on Immunization Practices (APIC) against the nasal vaccine. A paper in the Annals of Internal Medicine reported a cluster-randomized trial of the trivalent live attenuated nasal flu vaccine (nasal spray) versus the trivalent inactivated injected vaccine in 52 Hutterite communities in rural Canada over three flu seasons. The two vaccines were equally effective, with just over 5 percent of children in both groups contracting lab-confirmed influenza. These results contradict an earlier study, which prompted the CDC to advise against the use of FluMist. In that study, the nasal vaccine used was quadrivalent. Baylor College of Medicine Professor Pedro Piedra told NPR, “Many of us felt very strongly that the [live attenuated influenza vaccine] was a better vaccine than the inactivated for children, and the data supported that. But something happened when it became a quadrivalent vaccine.” [Annals of Internal Medicine, NPR, CDC]
Nigeria begins mass polio vaccination, after two cases were detected in the Northern state of Borno. Nigeria once accounted for half of all polio cases in the world, but marked two years without a wild polio case in September 2015. In recent years, vaccinators have been unable to reach hundreds of thousands of children because of the terrorist group Boko Haram, which could account for the outbreak. It could also be that eradication efforts dwindled after Nigeria had been marked off the list of endemic countries, which now includes only Afghanistan and Pakistan. Michel Zaffron, director of polio eradication at the World Health Organization, said, “It is not surprising that attention would slip after two years without a case.” Steve Cochi, an advisor to the U.S. Centers for Disease and Prevention, added, “You lose political commitment very quickly when a disease appears to have disappeared.” [Science, WHO]
WHO will reconvene an emergency committee on Yellow Fever as the outbreak in Angola threatens the DRC and Congo in late August or early September, to evaluate new information from affected countries and consider revised recommendations. The initial meeting of the emergency committee occurred in May, during which the WHO categorized the Angola outbreak as “a serious public health event that warrants intensified national action and enhanced international support” but not a global public health emergency. As of August 3, more than 190 suspected cases have been identified in Brazzaville, Congo, which is across the border from Kinshasa, Democratic Republic of the Congo. The WHO has launched a massive vaccination campaign in Kinshasa, one of the largest cities in Africa, and along a high-traffic corridor between Angola and the DRC. [CIDRAP, WHO]
Image via NIAID (CC BY-SA 3.0)











