August 26, 2019

FDA approves new drug for resistant tuberculosis. The US Food and Drug Administration (FDA) has approved a new drug developed by the TB Alliance, pretomanid, which will be combined with bedaquiline and linezolid to create a new oral regimen for drug-resistant tuberculosis (TB). Compared to current treatments, the new regimen will cut treatment length down from 18-24 months to 6 months and increase treatment success rates of drug-resistant TB by nearly 60 percent. However, there are concerns about the affordability and accessibility of the drug in low- and middle-income countries. [NPR Goats and Soda, The Hindu, Nature]
Antibiotic spraying ineffective at preventing citrus greening. A new study at the University of Florida found that oxytetracycline, an antibiotic approved by the Environmental Protection Agency (EPA) to fight citrus greening in Florida, is not effective at preventing the progression of the disease in citrus trees. Spraying trees with oxytetracycline was found to have no effect on the rate of progression of citrus greening. However, when oxytetracycline was injected into tree trunks, the presence of the bacteria that cause citrus greening decreased notably, although this method of administration is not approved by the EPA and is expensive to implement. [NY Times, APS]
Antibiotic resistance genes found in gene-edited cows. The US Food and Drug Administration (FDA) reviewed the genomes of two genetically dehorned (polled) cattle and identified antibiotic resistance genes in both of the calves studied. The genes were located close to the editing site and conferred resistance to neomycin/kanamycin and ampicillin. These findings are concerning as the resistance genes in the polled cattle cells can be transferred to bacteria. Because the researchers identified unnatural DNA in the calves which their developers previously denied, the FDA now has the power to regulate them. [bioRxiv,Independent Science News]
Global measles outbreak may foreshadow a resurgence of polio. In the midst of record-breaking measles outbreaks across the globe, experts are worried about the possible resurgence of polio. Polio efforts originally aimed to eradicate the virus nearly 20 years ago, and some fear that funding for these programs may soon run out. The Global Polio Eradication Initiative (GPEI) has developed a five-year plan to continue eradication efforts through 2023, which requires a total of $3.27 billion in funding. Experts advise that continued efforts are necessary, and strong investments will be cost-effective in the long run. [STAT]
Blood clotting factors fight MDR bacteria. Scientists at Sichuan University in China evaluated the effect of using blood clotting factors (coagulation proteins VII, IX, and X) to target drug-resistant Gram-negative bacteria. These clotting proteins have intrinsic antibacterial properties and are able to target the bacterial outer membrane, which is essential for the survival of the bacterial cell. The coagulation proteins studied significantly damaged the bacterial cell of E. coli and were effective at targeting infections caused by Pseudomonas aeruginosa and Acinetobacter baumannii in mice. [Nature Cell Research, Science Daily]
Fecal microbiota transplants as a therapy for MDR colonization. Researchers at the US Mayo Clinic in Minnesota conducted a systematic review of 21 studies that analyzed the effect of fecal microbiota transplantation (FMT) on the decolonization of patients with multidrug-resistant (MDR) organisms. The analysis included data from 151 patients, and results indicate an MDR eradication rate of 37.5 to 87.5 percent among patients who received FMT. The researchers also suggested that FMT has the potential to successfully prevent recurring MDR infections. [CMI]
Unnecessary antibiotic prescribing common for dental prophylaxis. Scientists from the University of Illinois at Chicago analyzed antibiotic prophylaxis prescriptions for over 168,000 dental visits between 2011 and 2015. Nearly 81 percent of antibiotics prescribed for infection prophylaxis before dental procedures were deemed unnecessary according to clinical guidelines. While it is estimated that dentists prescribe approximately 10 percent of antibiotics in the United States, dental practices are an important target for antibiotic stewardship efforts as dentists constitute the primary prescriber of clindamycin, an antibiotic associated with a high risk of Clostridioides difficile infection. [JAMA Network Open, Healio]
Post-prescription audit and review effective at reducing antibiotic use. The Infectious Diseases Society of America recommends core antimicrobial stewardship strategies, which include antibiotic preauthorization (PA) from a pharmacist and post-prescription audit and review (PPR) between the prescriber and provider following 72 hours of antibiotic therapy. To evaluate these recommendations, researchers conducted a clinical trial among 2692 patients in North Carolina between 2014 and 2015. The study found a reduction in overall antibiotic use during PRR (mean difference: -40.1 days of therapy per 1000 patient-days), but there was little change during PA (mean difference: 4.4). The researchers also deemed PRR more feasible and effective at identifying inappropriate antibiotic use, increasing direct interactions with providers, and de-escalating antimicrobial use than PA in community hospitals (p<0.001). [JAMA Network Open]
Infographic of the week. Although overall rates of methicillin-resistant Staphylococcus aureus (MRSA) infections are declining, MRSA blood infections are not.
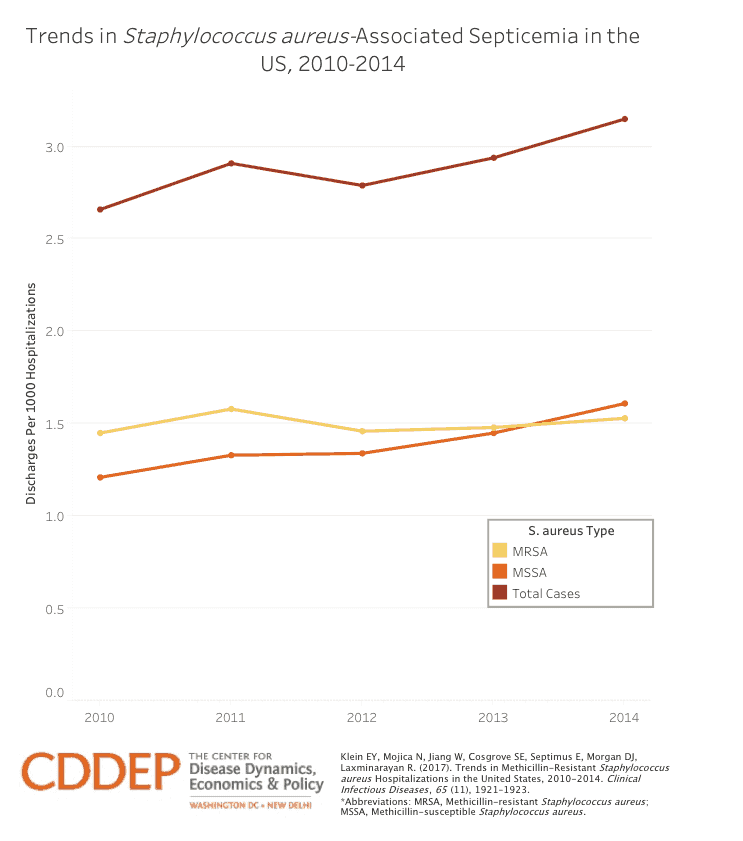
CDDEP researchers calculated rates of Staphylococcus aureus and MRSA-related hospitalizations from 2010 to 2014 and found:
- The rate of S. aureus septicemias increased nearly 20 percent, from 2.66 to 3.15 per 1,000 hospitalizations
- The rate of MRSA septicemias increased from 1.45 to 1.53 per 1,000 hospitalizations
- Methicillin-susceptible S. aureus(MSSA) septicemia increased from 1.21 to 1.61 per 1,000 hospitalizations [CDDEP]
Photo: Mycobacterium tuberculosis, Shutterstock











