February 10, 2017
A weekly roundup of news on drug resistance and other topics in global health.
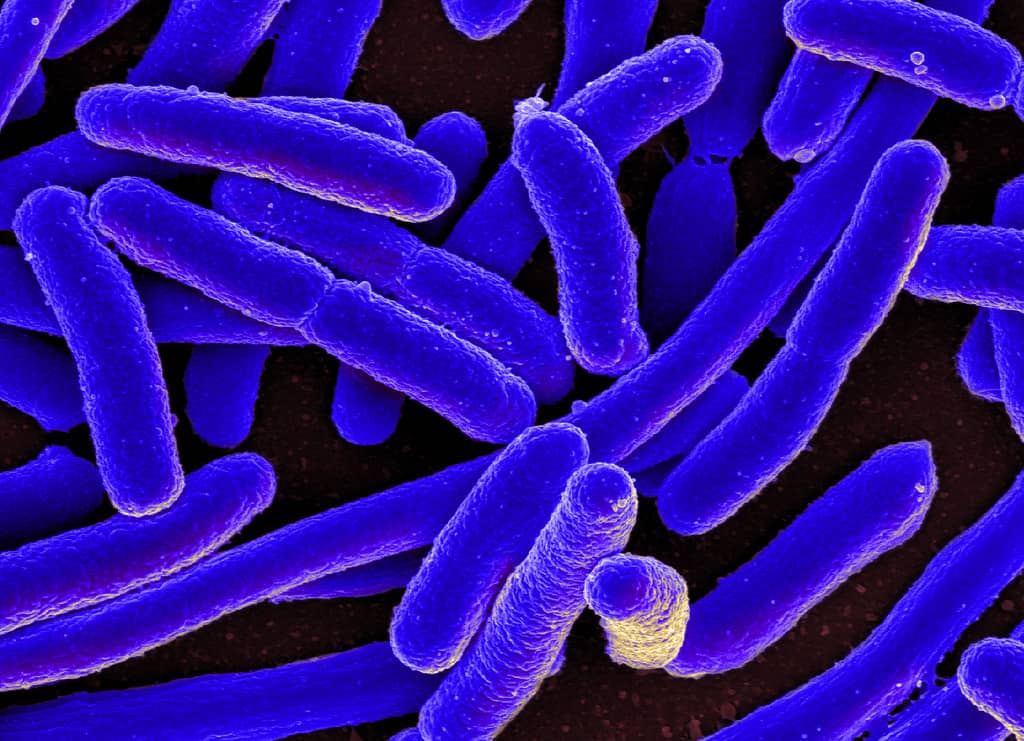
Bacterial tolerance may precede resistance. Resistant bacteria have genetically-controlled mechanisms that expel or destroy antibiotics, but “tolerant” bacteria can simply enter a dormant or slow-growing state in order to survive as antibiotics diffuse. In a study published in Science, researchers from The Hebrew University of Jerusalem exposed Escherichia coli to several rounds of ampicillin, which resulted in the bacteria developing resistance through ampC gene mutations. Reaching that state was a stepwise process, however, with a first mutation causing a growth slowdown, then the ampC mutation for ampicillin resistance. According to Professor Kim Lewis, from Northeastern University, who was not involved in the study, “Many people, including me, have been arguing that tolerance allows the pathogen to survive and live to fight another day… But what [the researchers] have shown is that when the resistance mutation occurs in the background of tolerance, the pathogen survives better.” [Science, The Atlantic]
Should you finish your antibiotic prescription? Experts have been questioning this longstanding advice, suggesting that some standard antibiotic regimens may be longer than necessary when signs and symptoms abate, and stopping treatment may be just as good for patients and better for the future of antibiotics. More and more research is examining strategies for shortening the standard duration of antibiotics to prevent unnecessary use. The World Health Organization (WHO) will discuss the issue next month at a meeting of the agency’s expert committee on the selection and use of essential medicine. [STAT, WHO]
Horizon Prize for rapid test to rule out need for antibiotics. The European Commission has awarded the €1 million Horizon Prize for better use of antibiotics to Minicare HNL for its finger prick test that can determine in less than ten minutes whether an upper respiratory infection is bacterial, and therefore whether or not the patient requires antibiotics. The test should be available for patients by 2018. Minicare HNL is a research and development partnership between P&M Venge AB and Royal Philips.
The first prize for the EU Health Award for NGOs fighting antimicrobial resistance was awarded to BEUC, the European Consumer Organization, for their campaign, “From Farm to You,” which has raised awareness of the unnecessary use of antibiotics in agriculture and its contribution to the rise of antimicrobial resistance. The second prize for the EU Health Award for NGO’s fighting antimicrobial resistance was awarded to the Alliance to Save our Antibiotics and third prize was awarded to WAAAR—The World Alliance Against Antimicrobial Resistance, a frequent CDDEP collaborator. [European Commission] [Revised 14 February 2017]
Cochrane Review: The most effective antibiotic stewardship interventions are underused. A Cochrane systematic review update of antimicrobial stewardship interventions found that enablement techniques—education, reminders, and prescription audits reliably improved the effectiveness of antibiotic prescribing restrictions, with particularly significant gains from audit and feedback, and goal-setting for physicians. But only 10 percent of the interventions tested used the most effective enabling strategies. According to lead author Professor Peter Davey, MD, of the University of Dundee School of Medicine, “We do not need more studies to answer the question of whether these interventions reduce unnecessary antibiotic use, but we do need more research to understand why the most effective behavior change techniques are not more widely adopted within hospital settings.” [Cochrane Review, press release, CIDRAP]
Inappropriate EAT therapy for bacteremia may increase recurrence and long-term mortality. A study published in BMC Infectious Diseases examining empiric antibiotic therapy [EAT] finds that appropriate EAT (defined as the first regimen started after a positive blood culture) for bacteremia, in which all blood isolates were susceptible to one or more of the antibiotics used, was associated with reduced recurrence and lower long-term mortality than a regimen not as well matched to the pathogen (inappropriate EAT). Of 6,483 patients studied, EAT was appropriate for 3,778 patients (58 percent) and inappropriate for 1,290 (the remainder were unrecorded). Short-term mortality was similar between the two groups, but long-term mortality (from one month to one year after treatment) was significantly higher in the inappropriate EAT group: 31 percent versus 22 percent. Recurrent infection was about 25 percent higher with inappropriate EAT. [BMC Infectious Diseases, CIDRAP]
Novel combination therapy may be key to overcoming resistance-conferring metallo-beta-lactamases. Findings published in Antimicrobial Agents and Chemotherapy demonstrate that adding aztreonam to the ceftazidime and avibactam combination used to treat multidrug-resistant Gram-negative infections could enhance its effectiveness against metallo-beta-lactamases. CIDRAP reports, “What [study author Robert Bonomo, MD] and his team hypothesized was that if aztreonam were added to the ceftazidime/avibactam combination therapy, the duo would help free aztreonam to work against infection-causing bacteria by protecting it from the other beta-lactamase enzymes, like offensive lineman in football blocking for a running back.” The combination treatment was successful in two patients, a 72-year-old woman with a multidrug-resistant bone infection and a young kidney transplant patient with bacteremia. [AAC, CIDRAP]
Recorded Webinar 2/7/2017 – Global Antimicrobial Stewardship: Barriers and Solutions. The Center for Infectious Disease Research and Policy (CIDRAP) hosted a webinar on global antimicrobial stewardship with infectious disease experts Dr. Debra Goff (USA), Dr. Dilip Nathwani, OBE (UK) and Dr. Marc Mendelson (South Africa). The webinar recording is available on YouTube. [YouTube]
Image via NIAID











