December 07, 2021
The pandemic, which highlighted the inequities of the American medical system, has morphed into a pandemic of the unvaccinated and is primarily occurring in rural America. Data from the CDC shows that the risk of dying from COVID-19 is 14 times greater among unvaccinated individuals compared to their vaccinated counterparts. Research also shows vaccination was 14 percent higher in urban areas than rural areas as of August 2021.
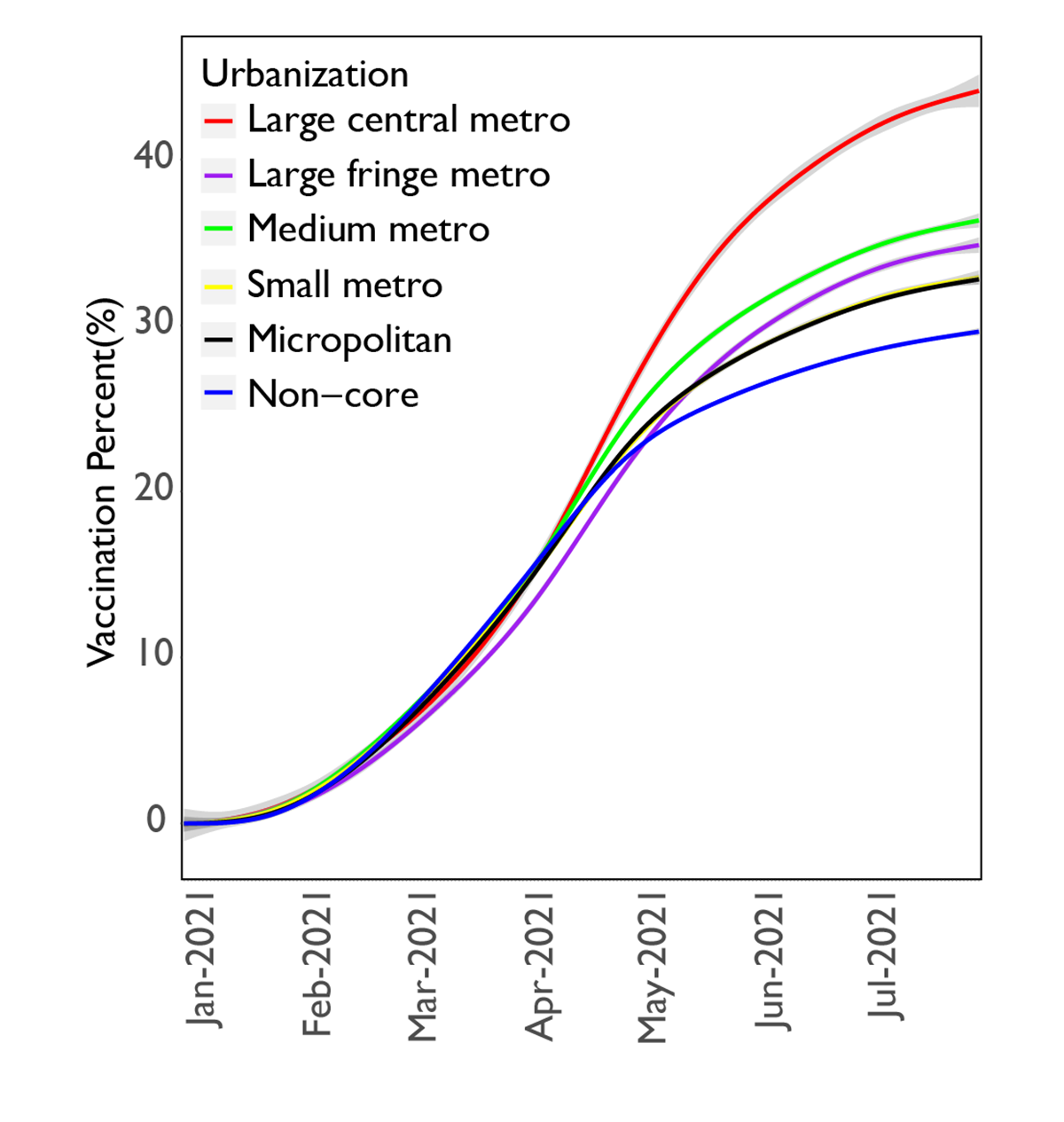
At the beginning of 2021, vaccinations increased rapidly across all urbanization levels. By July, differences in coverage rates became evident as vaccinations slowed more quickly in rural areas compared to urban areas. As restrictions were removed in early July and the Delta variant began spreading rapidly, the impact of differences in vaccination rates became crucially important, increasing the risk of COVID-19 related mortality among residents of more rural areas.
Recent studies on rural-urban and within-rural differences in COVID-19 vaccination rates show that higher levels of rurality are correlated with lower vaccination rates. To more effectively assess the risk of lower vaccination rates, we estimated vaccination and mortality rates in the fall of 2021 by level of urbanization as defined by the Census. The Census categorizes geographical areas into six urbanization levels from large urban areas (clusters of one or more counties that have an urban center with more than one million people) to rural areas (clusters of counties without cities of more than 10,000 people, called “noncore” as they are not defined by a core urban area).
| Urbanization Level | Definition |
| Metropolitan Counties: | |
| Large central metro | counties in MSA of 1 million or more population |
| Large fringe metro | counties in MSAs of 1 million or more population that do not qualify as large central |
| Medium metro | counties in MSAs of 250,000 to 999,999 |
| Small metro | Counties in MSAs of less than 250,000 population |
| Non-metropolitan Counties: | |
| Micropolitan | counties in micropolitan statistical areas |
| Non-core | nonmetropolitan counties that are not in a micropolitan statistical area |
Definitions extracted from the National Center for Health Statistics (NCHS)
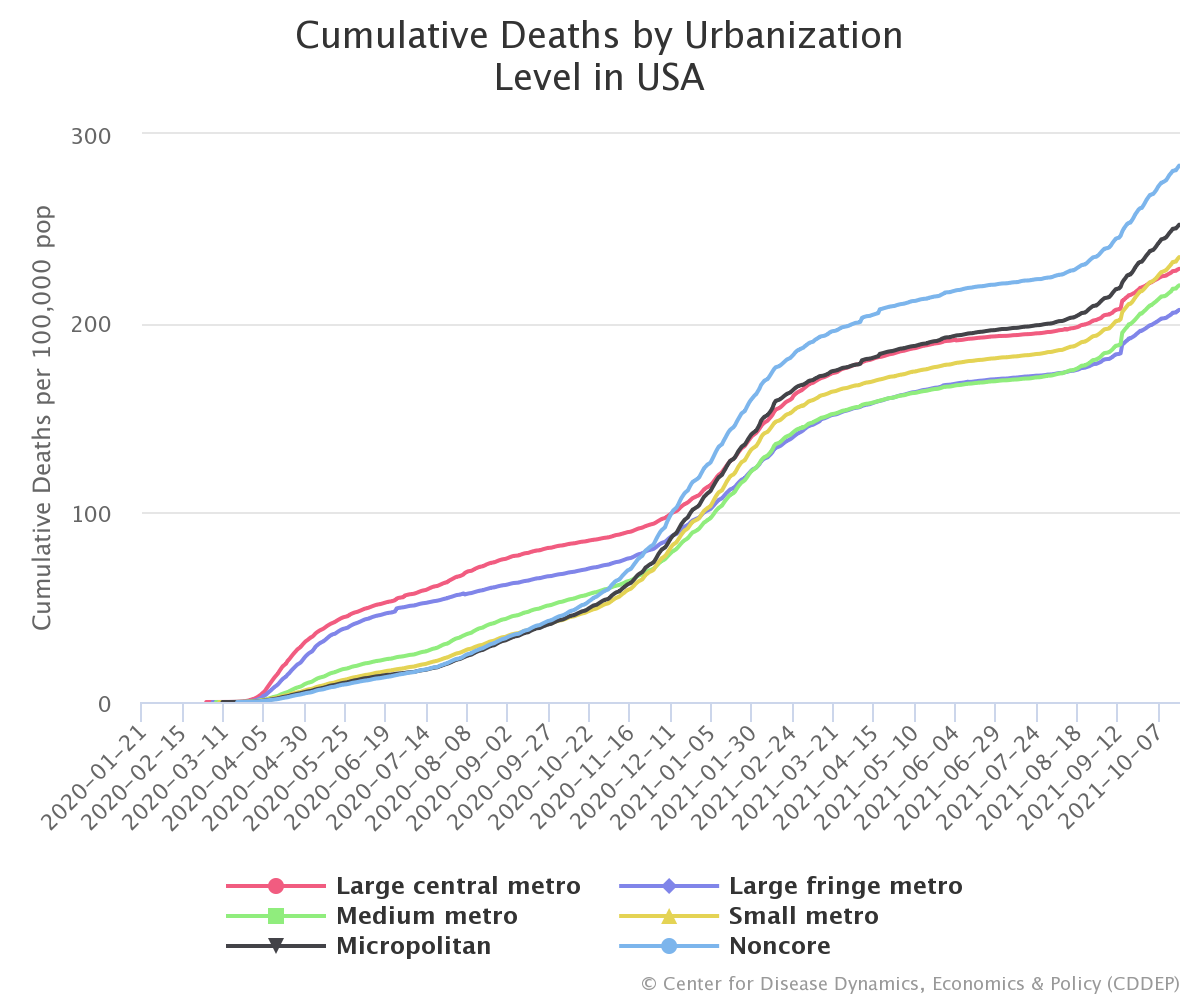
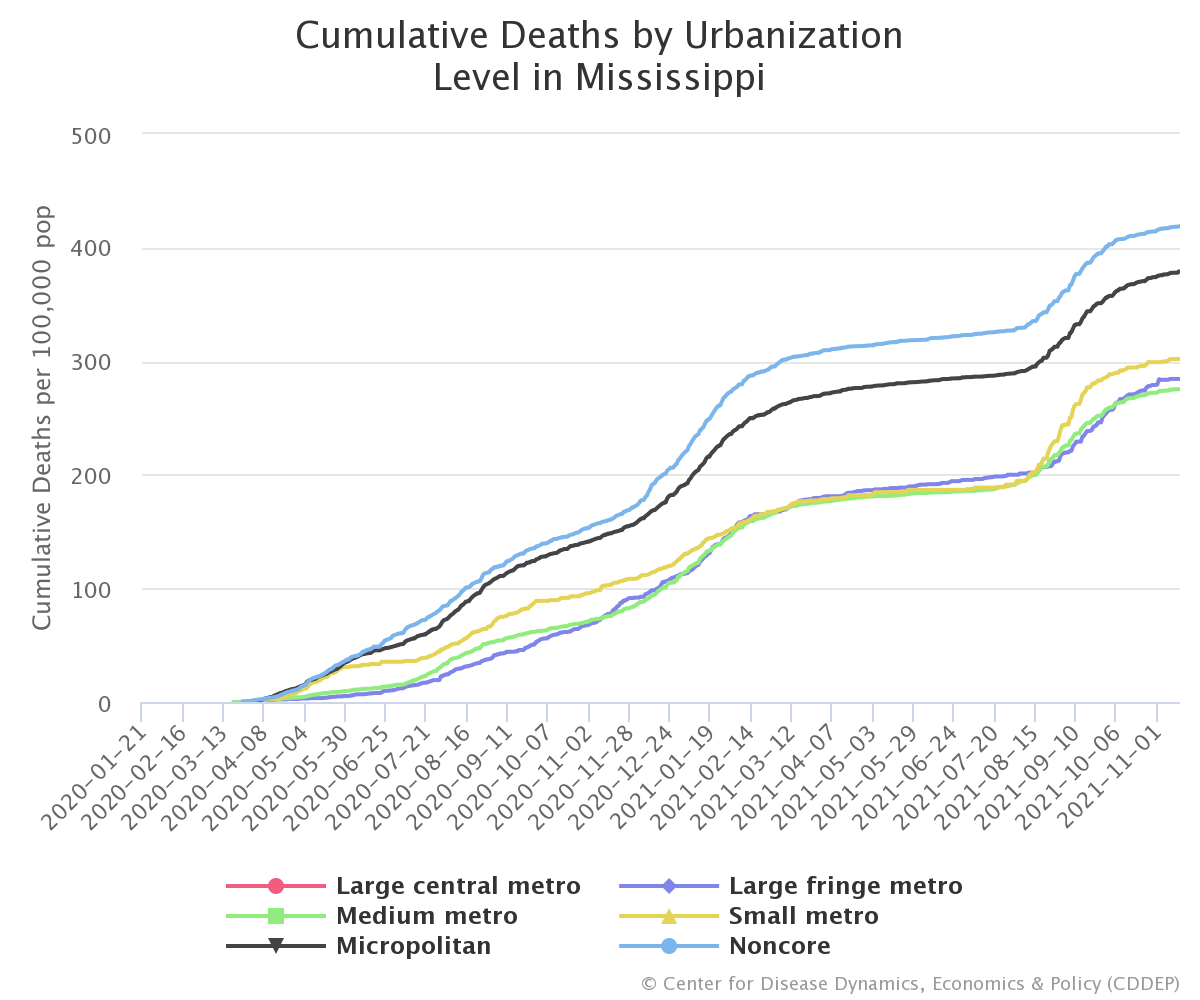
While the early part of the pandemic was centered in New York, Detroit, New Orleans, and other large urban centers, rural communities’ cumulative mortality rate (101 cumulative deaths per 100,000 population) surpassed large metro areas by early December 2020, even before the vaccine was available. By late January, 2021 micropolitan areas (counties with a city between 10,000-50,000) also surpassed large metro areas with 136 cumulative deaths per 100,000 population.
The mix of older populations with less access to health care combined with political messaging eschewing information on protective measures in rural areas were the likely reasons for the rising differences between mortality rates based on geography. With the arrival of the vaccine in late December 2020, however, the belief was that vaccinations would reduce mortality across all areas. However, although all US states made vaccines available for residents aged 16 and older by April 2020, the percentage of people vaccinated in more rural areas has lagged behind urban areas. As a result, the overall mortality rate in rural areas has increased faster compared to more urban areas. As of the end of November 2021, the mortality rate gap between noncore and large central metro areas had nearly tripled since the beginning of July, with the cumulative mortality rate increasing 43% in rural areas from 221 to 318 per 100,000, while only growing 24% in large central metros from 193 to 241 deaths per 100,000 population.
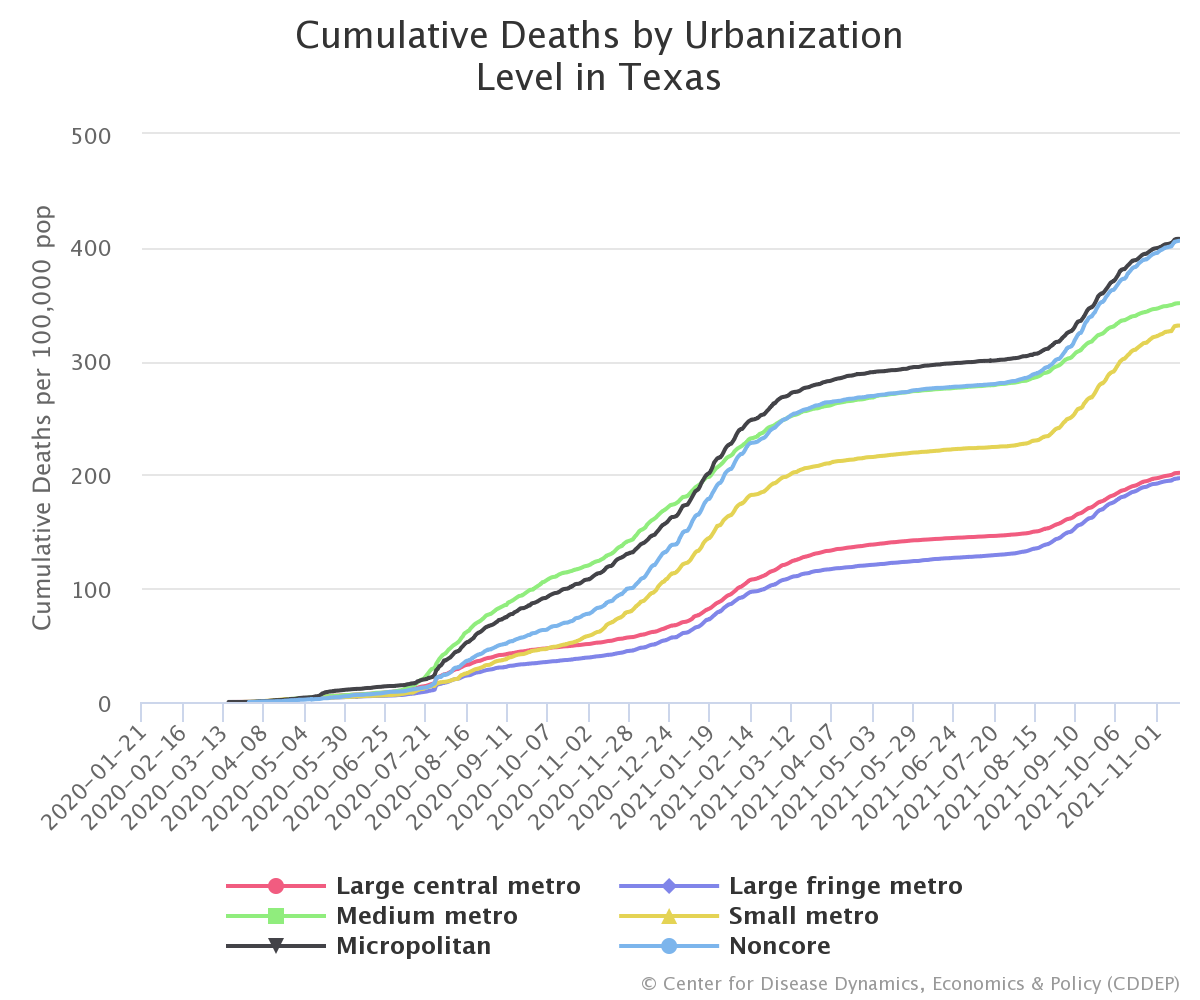
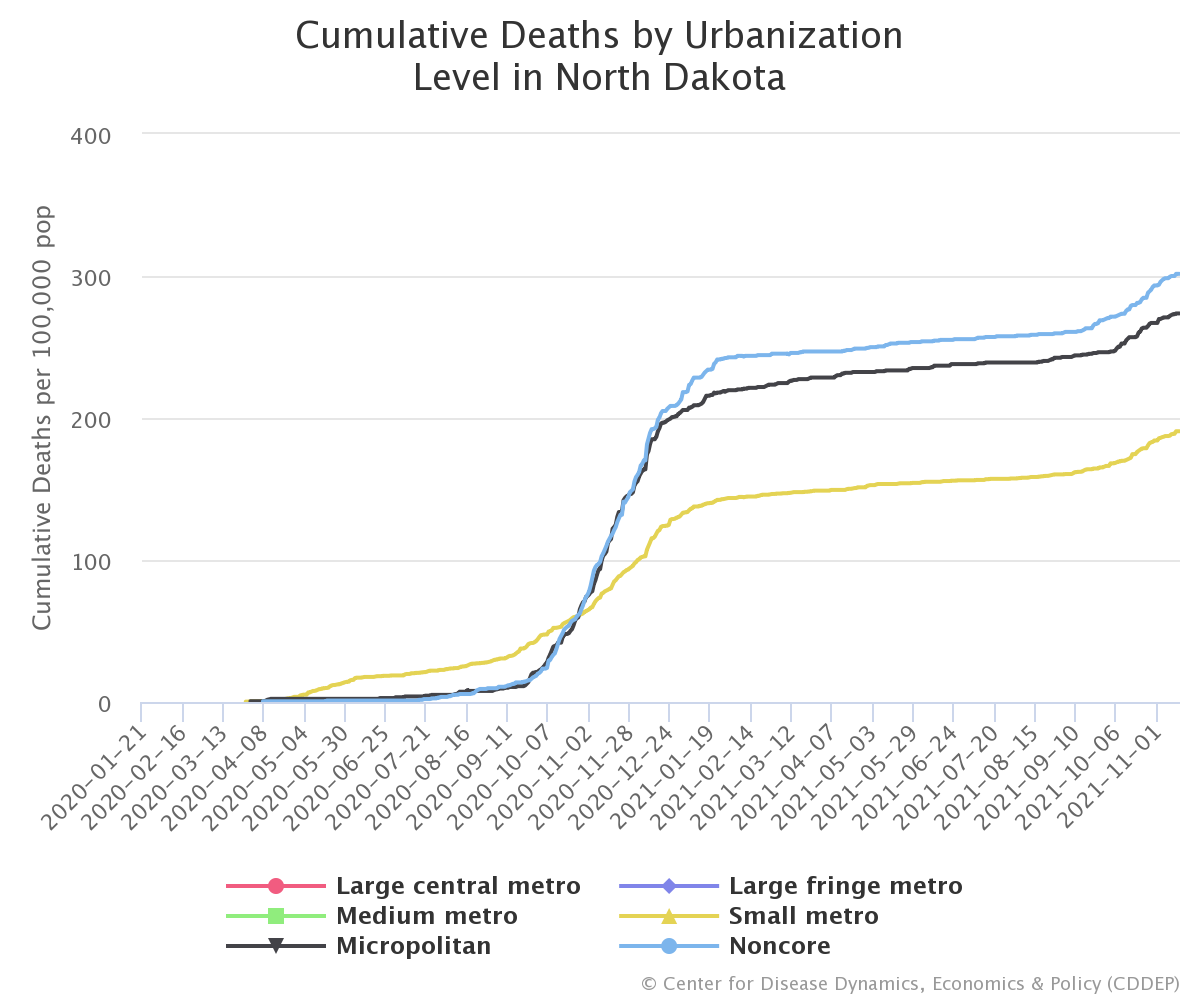
A closer look into individual states shows that the breakdown within states is even larger. In Texas, for example, cumulative deaths within micropolitan and non-core areas (412 deaths per 100,00 residents) more than double the rate in more metropolitan areas (205 deaths per 100,000). Additionally, smaller states with smaller urban cores, such as North Dakota and Mississippi, reveal similar trends with cumulative deaths in micropolitan and non-core areas surpassing those in more metropolitan areas.
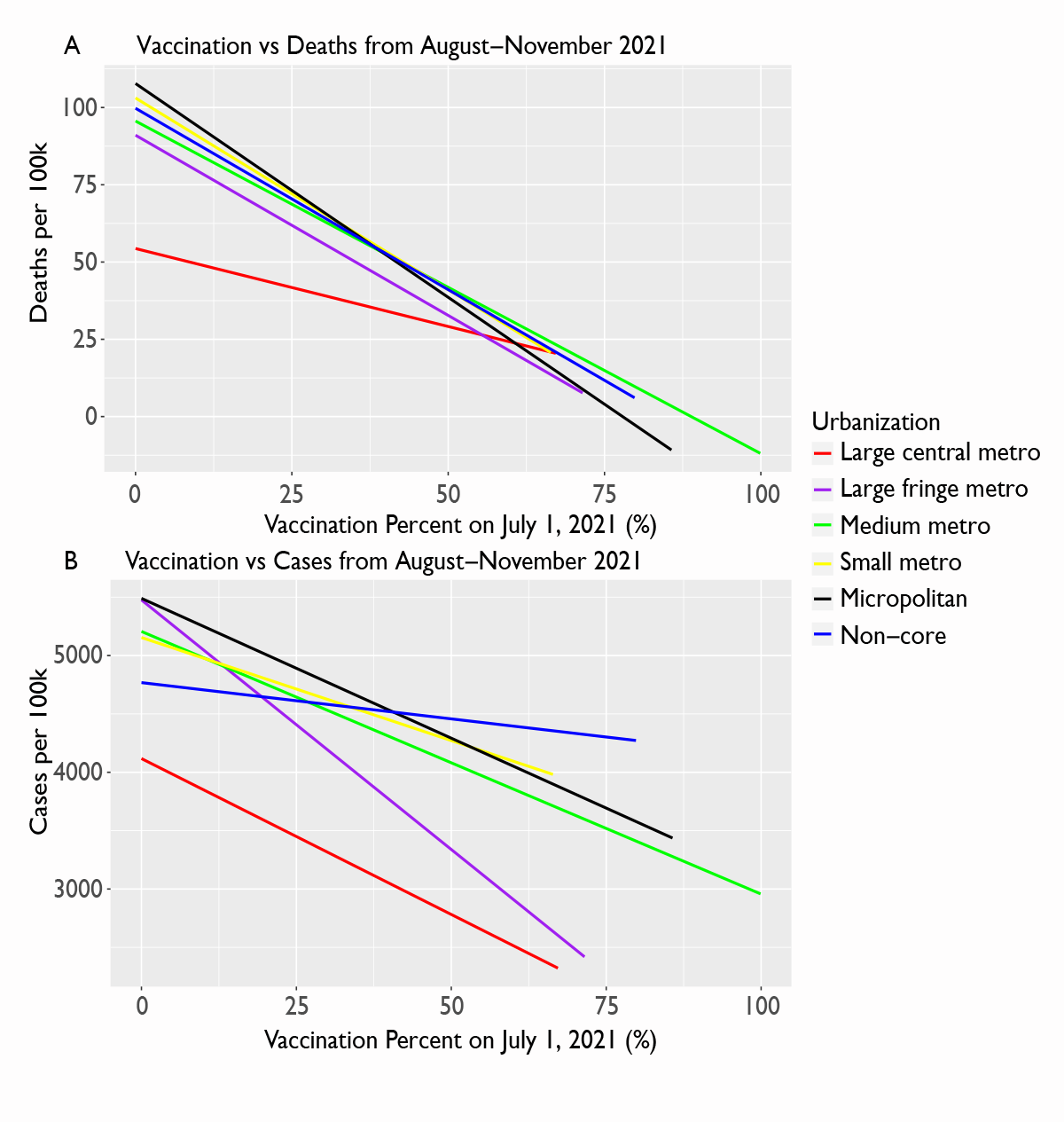
What is the likely impact then as new variants, such as Omicron, begin to appear? While evidence on the effectiveness of vaccines against the Omicron variant remains uncertain, based on the evolutionary epidemiology of other respiratory viruses, including other coronaviruses, the most likely scenario is that vaccine efficacy against severe disease, hospitalization, and mortality will remain high, but effectiveness against infection and symptomatic disease will be lessened. Similarly, reinfection rates among individuals previously infected are likely to increase. This suggests two important potential results (1) areas with high vaccination rates may not escape surges in cases, but mortality rates should remain lower, and (2) prior infection is unlikely to protect against reinfection, which means areas that have already seen surges are likely to see surges again this winter. The latter is problematic in areas with low vaccination rates as this increases the pool of individuals likely to end up with severe disease, putting pressure on hospital systems and leading to more deaths. Given that vaccination rates remain low in many rural areas when compared to more metropolitan areas, these areas may continue to have increased mortality rates. Unfortunately, the uptake of vaccination has become politicized. Future public health research should not only assess knowledge, attributes, and practices (KAP) of rural residents regarding COVID-19 vaccines, but also factors able to better influence and change existing public health campaigns and initiatives to reach these high-risk communities.











