In this episode, Dr. Nicholas White of the University of Oxford in the UK and Mahidol University in Thailand tells us how the world is losing ground in the fight against malaria, in no small part because of the emergence of resistance.
Malaria is caused by a parasite transmitted by mosquitoes, and these parasites have repeatedly evolved to escape the effects of drug after drug over the decades. Now, Dr. White argues, there’s a chance to get out ahead of this resistance. How?
Listen as he tells our host Maggie Fox how the parasite manages to evade the effects of drugs and what he thinks needs to be done to stop it from happening yet again.
Maggie Fox
Hello, and Welcome to One World, One Health with the latest ideas to improve the health of our planet and its people. I’m Maggie Fox.
The people of planet Earth are facing pollution, climate change, and new and reemerging infectious diseases. What can we do about them? This podcast is brought to you by the One Health Trust, with byte sized insights into ways people are trying to help.
In this episode, we’re chatting with Dr. Nicholas White, a professor of Tropical Medicine at the University of Oxford and at Mahidol University in Thailand. He’s been intensively studying a range of diseases, but especially malaria, and its growing resistance to the drugs used to treat it. The World Health Organization estimates 241 million people had malaria in 2020, and it killed 627,000 of them, mostly very young children. It’s caused by parasites that are carried by mosquitoes. People get infected when they’re bitten. And these parasites, which then live through complex life cycles in the human body, are hard to kill off. It gets even harder when they evolve resistance to the drugs used against them.
Nick, thanks for taking the time to talk to us about this problem.
Nicholas White
Pleasure.
Maggie Fox
Your work in recent years has especially focused on a class of drugs called artemisinin. Can you tell us a little about them?
Nicholas White
Yes, they are derived from a plant actually; they came into general usage via Chinese traditional medicine, which is an unusual route, and indeed, their entrance was unfortunately far too slow. In a nutshell, they are simply the most rapidly acting anti-malarial drugs that we have ever had. And they’re also remarkably well tolerated. So they form the backbone of nearly all anti-malarial treatment today.
So they come from an annual plant, which in English we call Artemisia Annua. In Chinese, it’s now called Qinghao. And the product of that is Jing Hao Tsu, which is the artemisinin from artemisinin, which is chemically slightly complicated; it’s called a sesquiterpene lactone peroxide, you can modify it slightly to make it more easily absorbed or more water-soluble, so you can give it by injection. So we use derivatives of artemisinin today. And we use them in two ways; one is mainly for treating uncomplicated malaria. So they use that in combination with another drug, the so-called artemisinin combination treatment, or ACT. And that’s the most widely used anti-malarial drugs in the world. And then for severe diseases where they reduce mortality, we give them by injection drug main called artesunate, is given by intravenous or intramuscular injection. And they are, as I said, remarkably effective drugs, they make people better more quickly than any other drugs, and they have almost no side effects.
Maggie Fox
So we’ve got these safe and effective drugs. What’s the problem?
Nicholas White
For most people, there isn’t a problem. But as ever with microorganisms, resistance has emerged. It’s been hard to develop resistance, but it has occurred now to all classes of antimalarial drugs. So the resistance to artemisinin was first noticed in the area of the world where I work: in Southeast Asia, near the Thailand-Cambodia border. And that was really recognized from about 2007 onwards, and it spread across the whole of that part of the world. We call it the Greater Mekong subregion.
And then, very worryingly, there were reports from other parts of the world, from South America, and most recently, and very worryingly from east Africa, around Uganda, Rwanda, that part of east Africa. And it’s very concerning, because Africa is where most of the world’s malaria occurs and where most of the deaths occur. So if we were to lose these drugs, it would be literally a disaster.
Maggie Fox
But I think you’ve come up with a solution to this problem of resistance. And it’s similar to some of the techniques used against antibiotic-resistant organisms. Isn’t that right?
Nicholas White
So I wouldn’t go as far as to say that we have a solution to artemisinin resistance, but we have a countermeasure, which should work at least for the short term. And that is to do what we do when we treat tuberculosis or HIV or some other infections. And that’s instead of combining two drugs, combining three drugs. So we’ve got several different partner drugs to the artemisinin that can be put together. And of course, it’s much harder now for the organism, the malaria parasite, to develop resistance simultaneously to all of these at once.
So these triple artemisinin combination treatments or TACTs should give us at least a few years of continued drug efficacy. Whilst we wait for the next generation of antimalarial drugs to be evaluated and deployed, which won’t be for quite a long time, unfortunately for several years. So we need to secure at least the short term. And I think we need to realize that it’s important to prevent resistance; it’s very hard to persuade people to act in advance. But somehow or other, I think we need to persuade the malaria community that we need to secure the future, not just the present by preventing resistance.
There are about 10 to the power 17 parasites in the world on any day. And that means that there are lots of opportunities for resistance mutations to emerge and the anti-malarial drugs are used very widely because malaria is ubiquitous; it’s so common in tropical countries that people take anti-malarial drugs all the time. So very quickly, after drugs were developed resistance emerged. The first resistance was to the antifols drugs like a proguanil, pyrimethamine, and then Chloroquine, which was a really good drug, and the mainstay of the first unfortunately failed attempt to eradicate malaria. That was used by the hundreds of metric tons a year, which meant that the average person in tropical countries had Chloroquine in the blood. Because Chloroquine is very slowly eliminated, has a half-life of about a month or terminal half-life.
So the selection pressure on malaria parasites was absolutely enormous. And unsurprisingly, eventually, resistance emerged. So Chloroquine resistance really started here again, in Southeast Asia, in fact, the same place that had artemisinin resistance developed and it spread, it spread across Asia and into Africa. It arrived in Africa about 1979 and had reached the western seaboard by about 1992. Independently resistance to Chloroquine emerged in South America. But the problem was the malaria community, are conservative, very slow to change. And unfortunately, despite the fact that Chloroquine didn’t work, it was still the main drug recommended across much of the tropical world until about the mid 2000s, when eventually, belatedly, policies changed. But the cost of this resistance was millions of deaths in children.
Maggie Fox
Can the parasite evolve resistance to this new triple therapy?
Nicholas White
I wouldn’t say we’re seeing the same resistance, no. What we’re seeing is a slowing of the rate at which the parasites are cleared from the blood. We are not seeing high-level resistance yet, fortunately. Now, by high-level resistance, I mean, that you have malaria, I give you the medicine, and you just get worse and sometimes die. That doesn’t happen. But we are definitely seeing the early signs of resistance where the parasites clear slowly from the blood. And because the artemisinin component of the ACT is protecting the other drug, then what we’ve seen in Southeast Asia is that the partner drug starts to fail.
So it’s a bit like dominoes, you know, the artemisinin goes, and then the partner drug goes. And so we’re very worried that we would see higher levels of resistance in the not too distant future. And also, because artesunate is so valuable in the treatment of severe malaria if we start to lose its advantage over the other drugs, which is what happens with resistance, then we might see mortality and severe malaria rising. So I wouldn’t say it’s as bad as it was for Chloroquine by the 1990s, which was disastrous, but it’s the first signs and as I said before, we’re very slow to respond to malaria. So we really need to do something now, before a big problem arises, rather than do what we’ve always done in the past, which is wait for an enormous problem to arise for deaths to go up, and then wait longer, and then eventually change. That’s not good.
Maggie Fox
Are you seeing the same reluctance to move away from the old way of doing things when it comes to using this new artemisinin triple therapy?
Nicholas White
I think conservatism is not necessarily a serious fault in medicine. But unfortunately, malaria is very, very slow to respond to worsening situations. Unfortunately, the malaria business, if you like, is now increasingly occupied by people who don’t really have much firsthand knowledge of the disease, don’t understand necessarily the biology of the parasite, more and more, or should I say less and less technical knowledge, unfortunately. And this conspires to prevent progress. So we’ve seen malaria in the world, effectively getting much better in the first 15 years of this millennium and then getting worse again.
So from 2015, progress has effectively halted. And we really need to do more. And that means we need to be proactive in preventing resistance. But yes, I’m afraid our community is very, very reluctant to change. And the really important idea, which is, I think a general idea in antimicrobial resistance, and that is, you need to prevent it, not to let it happen, and then try and stop it. That idea hasn’t really percolated through yet. People, unfortunately, still want to be confronted with the problem, and then try and solve it. And that’s not it. As we all know, for resistance, it’s much harder to deal with once it’s emerged. So we’re trying hard to persuade people to prevent it and not try… Put the fire, don’t let the fire start, rather than let it start and then try and put it out.
Maggie Fox
I know a lot of people see vaccination as the ultimate solution. The malaria vaccine has been especially intractable. How do you view the possibility of a vaccine as a solution to the problem?
Nicholas White
Yes, you’re right. It’s been very hard to develop a malaria vaccine. Not surprisingly, it’s in fact, the first vaccine against a parasite in humans. It’s hard to make vaccines against parasites. That’s also not surprising. The vaccine we’ve got, okay, it’s a sort of moderately good vaccine, not very good, not very bad. It provides short-term protection. I think it’s part of the solution, It’s probably a moderate-sized part of the solution. It’s certainly not going to sort the problem out. We are not going to eliminate malaria with a malaria vaccine. But a malaria vaccine will be very useful with other measures.
So the main measures, as you know, are vector control. So that means using insecticides judiciously and giving insecticide-treated bed nets in areas where they work, which is nearly everywhere. And then treating malaria properly, and often preventing it as well with interventions like seasonal malaria chemoprevention. But the vaccine on top of that, well, is an additional, valuable, drug-independent tool, but it’s not, at least the vaccines we have at the moment are not good enough to be the sole solution.
Maggie Fox
Nick, thanks so much for taking the time to talk to us. This is a huge problem, and we really appreciate your insights.
Nicholas White
It’s a pleasure.
Maggie Fox
Listeners can share this podcast which is brought to you by the One Health Trust by email, Twitter, or your favorite social media platform. And let us know what else you’d like to hear about at [email protected]. Thanks for listening.
Guest
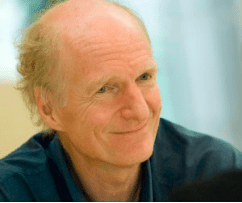
Professor Sir Nicholas John White FRS is Professor of Tropical Medicine at the Faculty of Tropical Medicine, Mahidol University, Thailand, and at Oxford University, UK. He is also a Consultant Physician in acute general medicine at the John Radcliffe Hospital, Oxford. Professor White is a Wellcome Trust Principal Research Fellow who chairs the Wellcome Trust Tropical Medicine Research Programmes in South East Asia. His main research focus is the pathophysiology and treatment of malaria. He has authored over 1,100 scientific publications and 50 book chapters. He has received the Prince Mahidol Prize for Medicine, the Canada Gairdner Foundation Global Health Prize, and the Royal Society of Tropical Medicine and Hygiene Manson medal. He co-chaired the WHO antimalarial treatment guidelines committee for twelve years and currently chairs the Scientific Advisory board of the Drugs for Neglected Diseases initiative and the COVID-19 Clinical Research Coalition.
Credits
Hosted and written by Maggie Fox
Special guest: Dr. Nicholas White
Produced and edited by Samantha Serrano
Music composed and sound edited by Raquel Krügel
Transcript created by Harsh Pingle